What is the difference between laser and radiofrequency procedures for varicose veins?
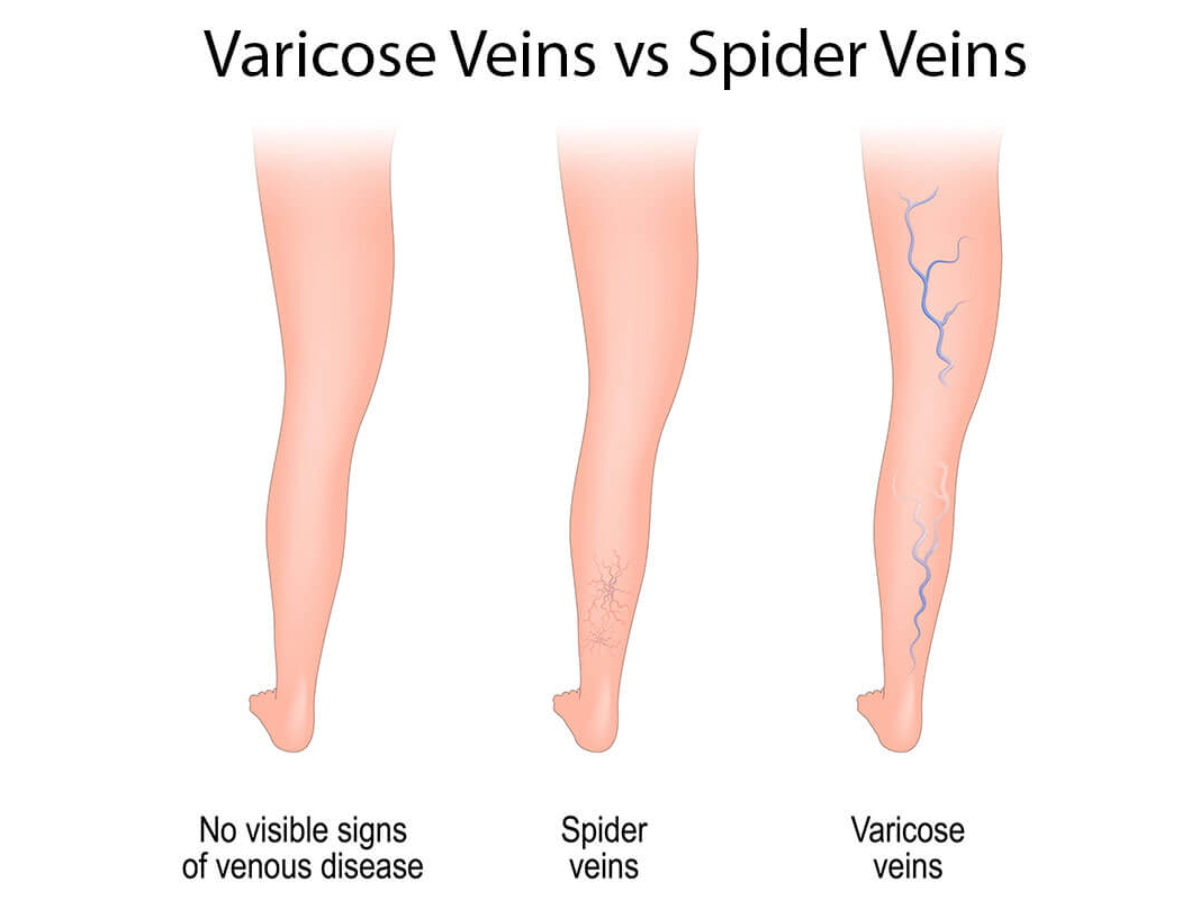
Both laser and radiofrequency ablation techniques are used as an alternative to surgery for the treatment of varicose veins and underlying venous insufficiency. The concept behind both laser and radiofrequency treatments is that an energy source is used to heat the vein, causing it to collapse and seal shut. Over time, the treated veins will dissolve. This is offered as an alternative to surgical removal of the veins. The basic difference between the two, are the types of energy sources used.
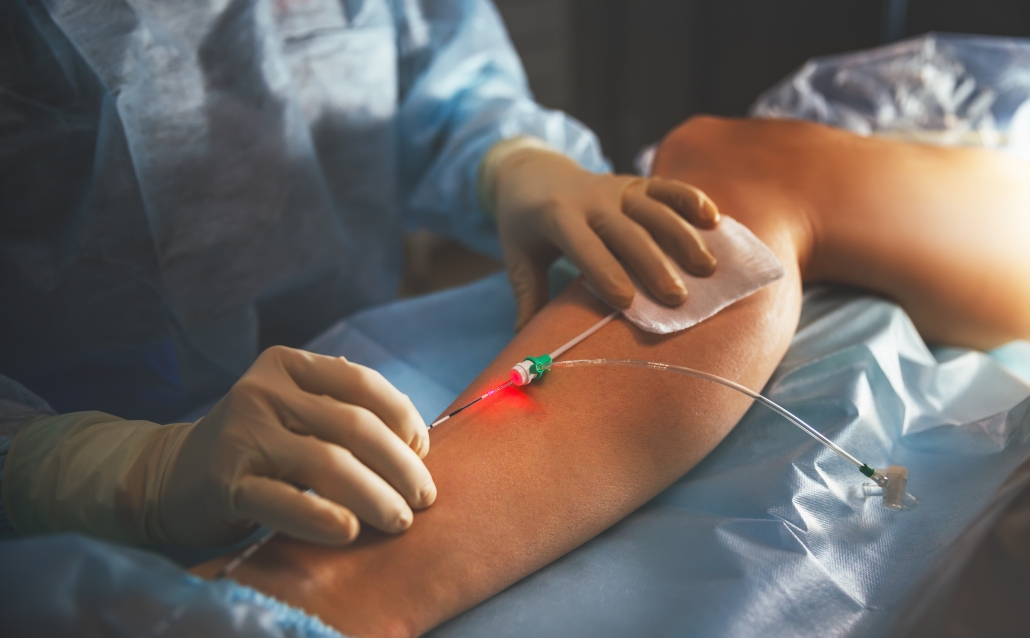
Laser vein treatment, also known as laser ablation or endovenous laser ablation therapy (EVLT or EVLA) utilizes laser energy to heat the vein.
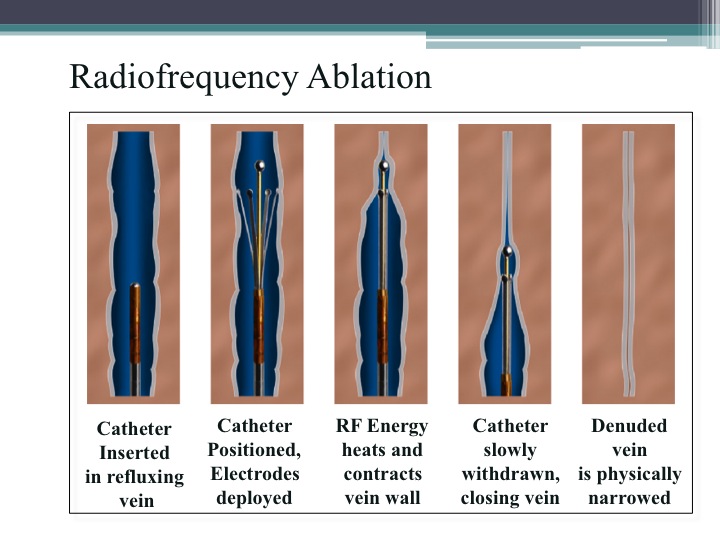
Radiofrequency vein treatment, also known as radiofrequency ablation (RFA), or the Venefit procedure (previously known as VNUS Closure) utilizes radiofrequency energy to heat the vein.
Both procedures are used to treat the small, great or anterior saphenous veins.
Either procedure involves making a tiny incision the size of a grain of rice on the skin, and a narrow catheter is inserted into the vein. The machine applies either laser or radiofrequency energy to the vein interior, an action that heats the vein and seals it closed.
Unlike traditional surgery, this new minimally invasive procedure takes about 30 minutes to perform and patients can walk out of the office afterward.
While both are effective options for vein treatment, we prefer radio-frequency ablation over laser because it has been proven to be more comfortable than laser yet equally effective. It is also our experience that there is less bruising, pain, and quicker recovery associated with radio-frequency closure of the veins.

Laser vein treatment, also known as laser ablation or endovenous laser ablation therapy (EVLT or EVLA) utilizes laser energy to heat the vein.
Radiofrequency vein treatment, also known as radiofrequency ablation (RFA), or the Venefit procedure (previously known as VNUS Closure) utilizes radiofrequency energy to heat the vein.

The radiofrequency catheter is inserted inside the vein. Radiofrequency energy then heats the vein causing it to collapse and seal shut. We prefer radiofrequency over laser vein treatment because we find that it is more comfortable for the patient with less bruising.
Remember, that more than one treatment type is often needed such as radiofrequency of the saphenous vein + sclerotherapy of superficial branches. Talk to your doctor to find out which is best for you or schedule a consultation at 858-550-0330.