What is Vascular Disease?
LJVascular2022-03-23T11:47:16-07:00What is Vascular Disease?
Your body contains an amazing, intricate system of arteries and veins. Arteries bring oxygen-rich blood from the heart to every inch of the body; veins return the blood back to the heart and lungs for more oxygen.
Most people know that heart disease can occur when blood vessels become clogged with plaque and cholesterol, but many are unaware that the same problem, often called hardening of the arteries (or atherosclerosis), can occur in any artery of the body.
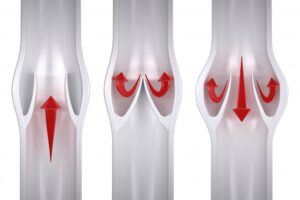
Venous problems occur in the veins, often resulting in leg swelling, deep vein thrombosis (blood clots) and chronic leg problems.
Common types of artery disease include:
Carotid artery disease and stroke
Carotid arteries in the neck bring oxygen to the brain. Patients who have had a stroke, a transient ischemic attack
(TIA) or have been told they have an abnormal sound in that artery, will be referred to a vascular surgeon for diagnosis and possible treatment.
Aneurysms
Aneurysms are bulges that develop in a weakened part of an artery. While these can occur in the brain, they are most common in the aorta, which is the body’s biggest artery, running from the heart through the abdomen. Aneurysms can also occur in the pelvis or the knee. They can enlarge when the heartbeat pushes against the weakened wall. In the aorta and pelvis, ruptured aortas can be fatal.
Peripheral arterial disease (PAD)
Patients with hardening of the arteries start to lose blood flow to the limbs. Early on, this may cause pain when walking, but as the disease progresses, it can cause painful foot ulcers, infections, and even gangrene, which could require amputation. People with PAD are three times more likely to die of heart attacks or strokes than those without PAD.
Common Vascular Disease Problems:
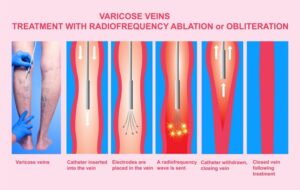
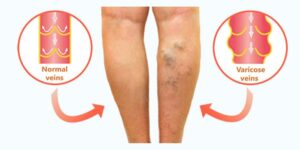
- Varicose veins which are often cosmetic, but can also be a sign of a more serious venous disease.
- Chronic venous insufficiency is a potentially painful condition that is caused by blood reflux or clotting.
- Deep vein thrombosis a blood clot in a deep leg vein.
Who are Vascular Surgeons:
Vascular surgeons train in vascular disease for five to seven years after medical school. Board certified vascular surgeons can treat any vascular condition with any treatment—medication, minimally invasive endovascular surgery, or open surgery. Many vascular conditions are lifelong, and your vascular surgeon may become a lifelong care partner. Be sure to ask to be referred to a board certified vascular surgeon.