What can I expect from Ultrasound-Guided Foam Sclerotherapy?
LJVascular2024-03-06T13:50:29-08:00Navigating Vascular Health: Understanding Ultrasound-Guided Foam Sclerotherapy
Ultrasound-Guided Foam Sclerotherapy: Elevating Vein Health
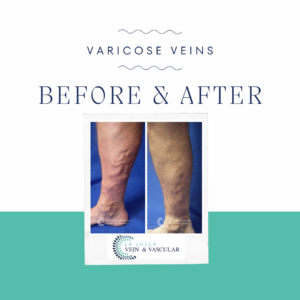
When addressing both visible varicose veins and those unseen by the naked eye, the efficacy of ultrasound-guided foam sclerotherapy becomes evident. This advanced procedure combines precise administration with ultrasound visualization, providing a safe and effective solution for various vein conditions. In this piece, we’ll explore the intricacies of ultrasound-guided foam sclerotherapy, the role of polidocanol (Asclera®), treatment frequency, and what to expect during your treatment sessions.
Unveiling Ultrasound-Guided Foam Sclerotherapy: A State-of-the-Art Solution
Ultrasound-guided foam sclerotherapy utilizes technology and medical expertise to target varicose veins that may not be immediately visible. Guided by ultrasound, the foam medication is precisely directed towards these veins. This technique effectively addresses veins near the skin or nerves and navigates complexly twisted veins.
Polidocanol (Asclera®): A Preferred Sclerosant
Polidocanol, known under the brand name Asclera®, stands out as a preferred choice among sclerosant medications. Its patient comfort and minimal risk of side effects make it a prime option for treatment. As a detergent-type medication, polidocanol gently disrupts the inner lining of veins, halting blood flow and eventually leading to vein closure. Approved by the FDA since 2010 for varicose vein treatment, polidocanol has a substantial success record in Europe for decades. Although the transformation of polidocanol into foam for treating larger veins is an off-label use, it has proven remarkably effective and well-tolerated by patients. Our experts at La Jolla Vein Care have extensive experience in foam sclerotherapy, ensuring capable hands for your vein health.
Treatment Frequency: A Tailored Approach
The number and frequency of treatments vary depending on individual anatomy, vein response, and patient goals. Typically, 2 to 5 treatment sessions achieve an 80% improvement. Some larger or stubborn veins may require multiple sessions for a complete response.
Your Treatment Days: Guided Steps Toward Vein Wellness
Preparing for your ultrasound-guided foam sclerotherapy session is simple:
Consent and Attire: You’ll sign a consent form and change into provided shorts.
Skin Preparation: Alcohol will cleanse your skin, and ultrasound will locate the veins for targeted treatment.
Injection Process: The foam medication will be injected into your veins using a fine needle, guided by ultrasound.
Recovery Period: Elevate your legs on a comfortable wedge pillow for about 15 minutes post-treatment.
Compression Stockings and Walking: After treatment, compression stockings will be applied, and you’ll walk for 30 minutes before leaving. Post-treatment, some achiness and tenderness may occur.
Ultrasound-guided foam sclerotherapy propels improved vein health by offering precision and effectiveness. At La Jolla Vein & Vascular, our committed medical team provides personalized care for your vein health journey. By embracing advanced techniques like ultrasound-guided foam sclerotherapy, you’re setting course for healthier, pain-free legs and elevated well-being.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!