Understanding Venous Disease: Beyond Myths and Realities
LJVascular2023-12-26T14:38:49-08:00Understanding Venous Disease: Beyond Myths and Realities
Venous reflux disease, known by various names like venous stasis, venous insufficiency, or venous incompetence, is a complex condition that impacts the veins in the legs. This article aims to unravel the intricacies of venous reflux disease—its causes, symptoms, and its progressive nature. Additionally, we’ll delve into the pivotal role played by ultrasound technology in diagnosing this condition and formulating personalized treatment plans.
Deciphering Venous Reflux
Venous reflux disease is centered around the concept of ‘leaky valves’ within leg veins. These valves, responsible for maintaining proper blood flow, may malfunction, leading to the backward flow (reflux) of blood instead of its intended route towards the heart. This reflux can affect both deep and superficial leg veins, hampering efficient blood circulation.
Unveiling the Anatomy of Reflux
Leg veins can be categorized into two main types: deep and superficial. Deep veins, nestled within the muscles, primarily transport blood from the legs back to the heart. Meanwhile, superficial veins reside just beneath the skin, playing a significant role in this condition. Notably, the Great Saphenous Vein (GSV) coursing through the thigh and calf, along with the small saphenous vein along the back of the calf, are key players in superficial vein issues.
Impact of Leaky Valves
Normally, one-way valves in leg veins assist blood flow against gravity, aided by the contraction of calf muscles. When these valves malfunction, blood backflows, resulting in pooling in the lower legs. This leads to symptoms such as leg heaviness, pain, fatigue, ankle swelling, and even restless legs at night. Over time, this condition progresses, leading to skin changes like darkening, dryness, itching, and the potential development of venous leg ulcers.
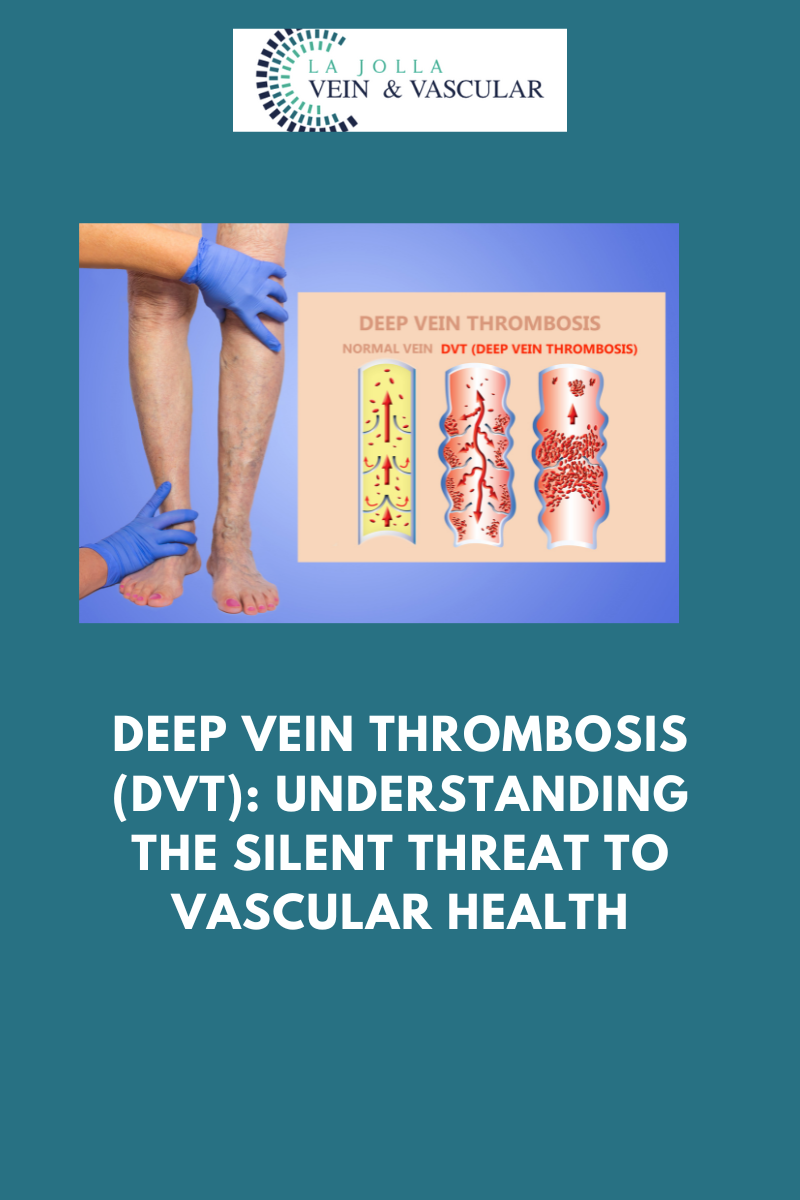
Diagnosis through Ultrasound
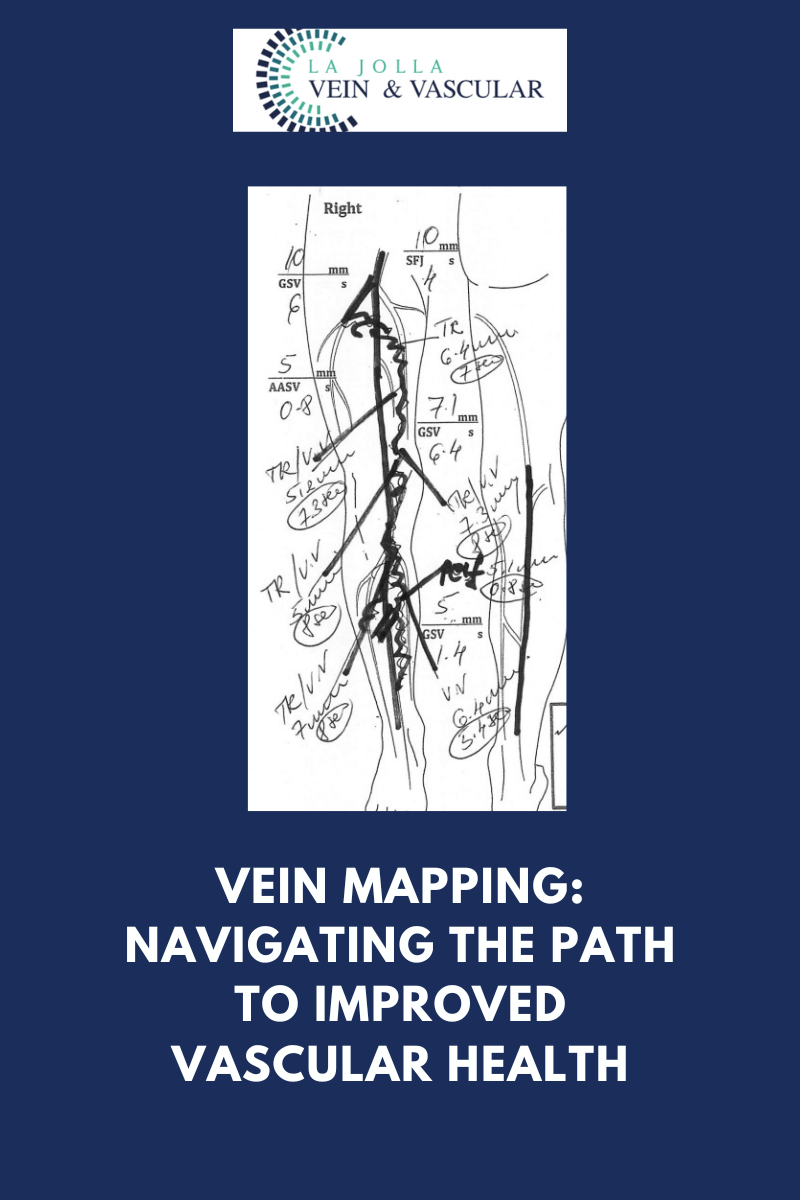
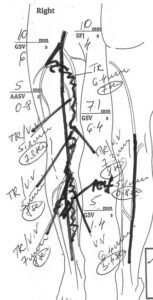
The diagnosis of venous reflux disease demands specialized tools, with ultrasound technology being pivotal. Many vein issues aren’t visible to the naked eye, as they arise beneath the skin’s surface. Ultrasound examinations provide insights into blood flow direction, valve functionality, and the presence of blockages or scars in the veins.
Personalized Treatment Approach
Effectively managing venous reflux disease involves a tailored strategy for each patient. The treatment typically involves three key steps:
Step 1: Addressing Underlying Reflux
Treatment starts with addressing the root cause—venous reflux—often focusing on the saphenous veins. Innovative vein ablation procedures like radiofrequency ablation, laser ablation, mechanico-chemical ablation (MOCA), and Varithena Foam are employed to restore proper blood flow.
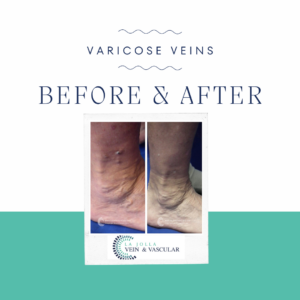
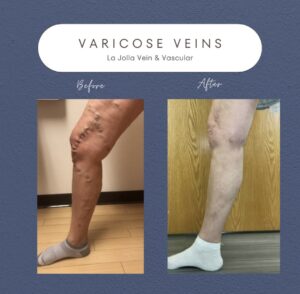
Step 2: Handling Varicose Veins
Once the underlying reflux is resolved, the focus shifts to varicose veins. Foam sclerotherapy or minimally invasive removal methods are employed to eliminate bulging veins.
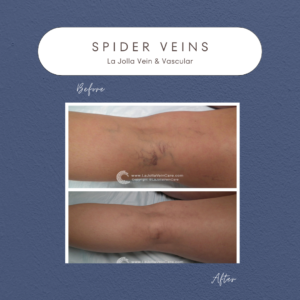
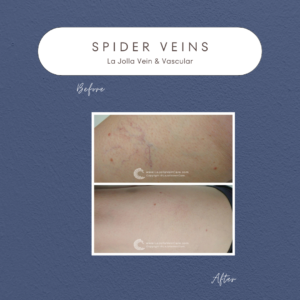
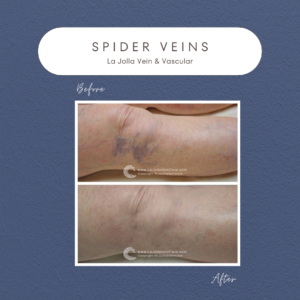
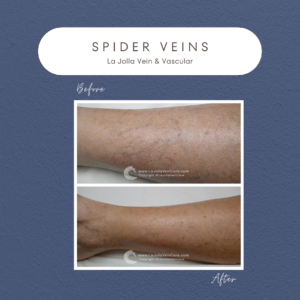
Step 3: Managing Spider Veins
For those seeking cosmetic enhancement, spider vein treatment through sclerotherapy completes the comprehensive treatment journey.
Venous reflux disease demands specialized care for effective management. Our approach encompasses cutting-edge diagnostics, advanced treatments, and personalized care to address the diverse aspects of this condition. Through our expertise and commitment, we strive to provide transformative outcomes that enhance both the health and quality of life of our patients. If you’re ready to embark on the journey towards healthier veins, reach out to us to take the first step towards comprehensive vein and vascular wellness.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!