A Glimpse into Varicose Veins: Unveiling the Transformation Journey
LJVascular2023-10-10T18:43:01-07:00A Glimpse into Varicose Veins: Unveiling the Transformation Journey
Varicose veins, those twisted, and bulging veins that often grace the surface of the skin, are a concern shared by many individuals. While their frequent appearance is in the legs, they can also manifest in other areas of the body. In this blog post, we embark on a journey into the realm of varicose veins. We’ll unravel their nature, delve into the root causes behind them, and illuminate the array of treatment options available for those who seek relief.
Defining Varicose Veins
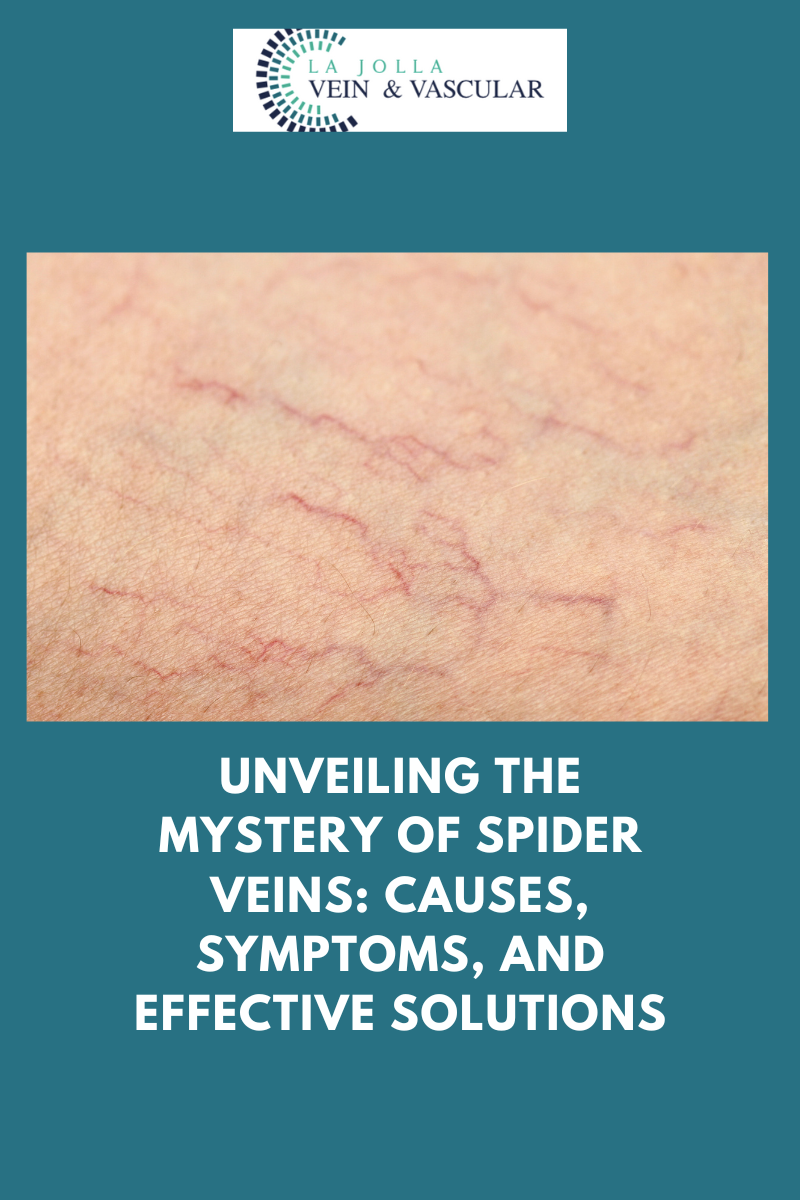
Varicose veins are the visible result of veins beneath the skin’s surface becoming swollen and distorted. While they may seem alarming, they are, in fact, a common condition experienced by many. The impact of these veins often extends beyond their appearance, causing discomfort, pain, or a lingering sensation of heaviness in the legs.
Unraveling the Causes
At the heart of varicose veins lies the issue of faulty vein valves. These valves play a pivotal role in maintaining the proper flow of blood by facilitating its journey toward the heart and preventing it from settling and pooling in the veins. The dysfunction of these valves gives rise to the accumulation of blood in the veins, leading to their gradual expansion. This condition is frequently associated with venous reflux disease, which goes by various names such as venous stasis, venous insufficiency, or venous incompetence.
Deciphering Venous Reflux
Venous reflux is the culprit behind the backward flow of blood, countering the natural pull of gravity due to the malfunctioning valves. Typically, the calf muscles aid in pumping blood upward, but in the presence of leaky valves, blood tends to collect in the lower legs. This pooling results in the visible bulging of the veins on the surface. This condition predominantly affects the great and small saphenous veins, the primary carriers of blood from the legs back to the heart. In more than 90% of cases, varicose veins in the legs are intricately linked to these veins.
Research Insights
A notable study, spearheaded by Dr. Nisha Bunke and documented in the Journal of Vascular Ultrasound in 2018, examined over 1,000 legs afflicted by varicose veins. The research unveiled the great and small saphenous veins as the primary culprits behind varicose veins in the majority of instances. Both the Great Saphenous Vein (GSV), meandering through the middle of the thigh and calf, and the Small Saphenous Vein (SSV), tracing its path along the back of the calf, were prominently implicated.
Pathways to Relief
The good news is that varicose veins are far from an insurmountable condition. Advances in medical technology and the realm of knowledge have paved the way for a spectrum of treatment options to alleviate discomfort and enhance the aesthetics of affected veins. Various minimally invasive procedures, including laser ablation, radiofrequency ablation, and sclerotherapy, have established their effectiveness in treating varicose veins.
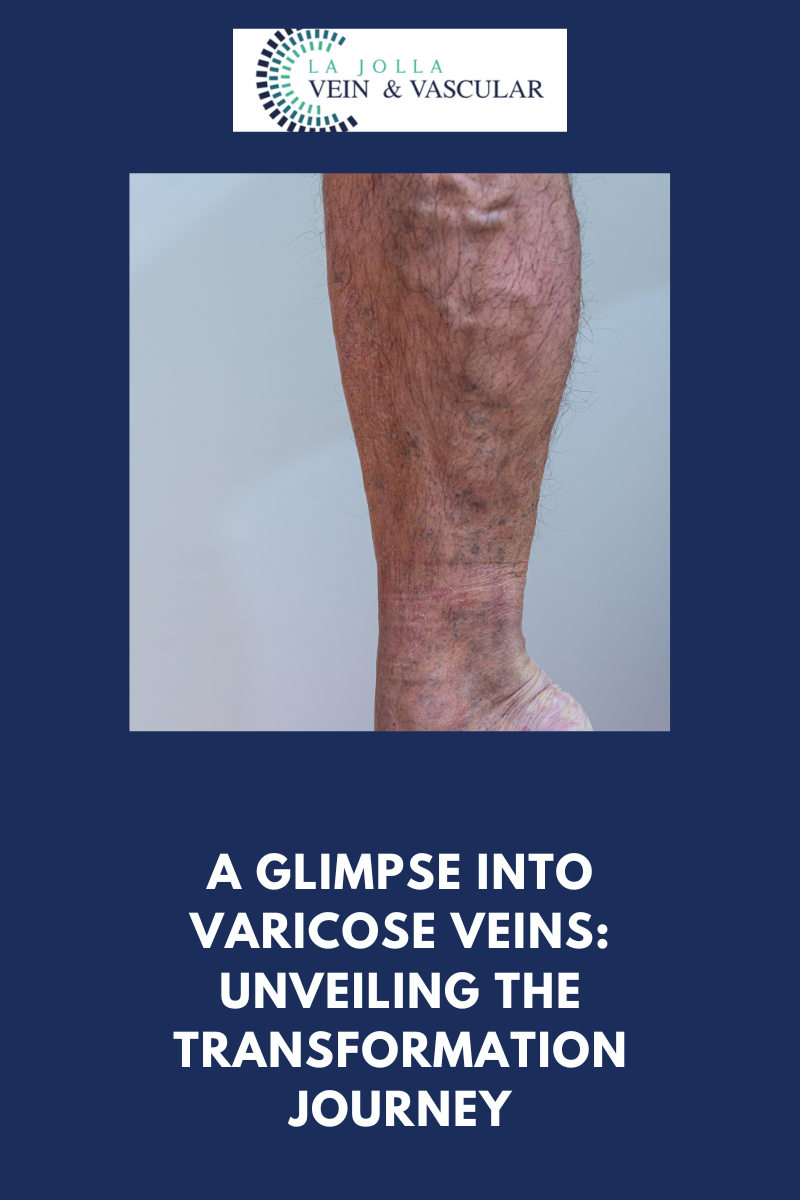
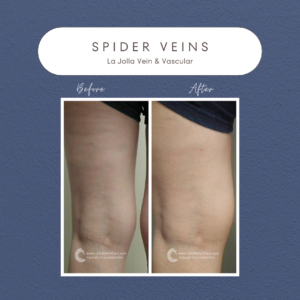
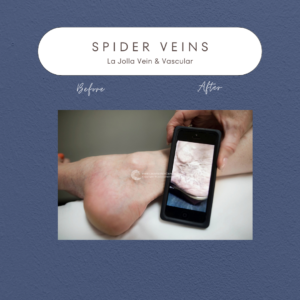
The Transformation: Before and After
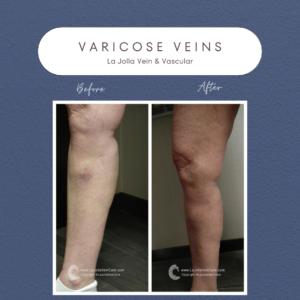
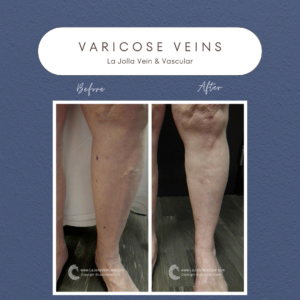

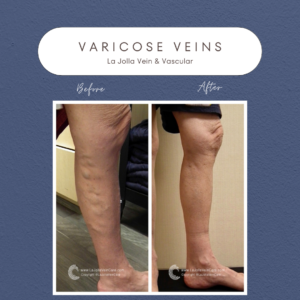
Witnessing the results of varicose vein treatment is nothing short of remarkable. Many individuals experience significant improvements in both the appearance of their varicose veins and the associated symptoms. These before-and-after images bear witness to the profound positive impact that proper treatment can have on one’s vascular health and overall well-being.
Varicose veins may be a prevalent condition, but armed with knowledge about their causes and treatment options, individuals can seize control of their vascular health. Modern medical techniques empower those grappling with varicose veins to seek relief and embark on a transformative journey toward an improved quality of life. Whether you are unraveling the mysteries of faulty vein valves, exploring the intricacies of venous reflux, or considering the various treatment avenues, the path to healthier veins commences with education and awareness.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!