Charting Your Course to Vascular Wellness: A Comprehensive Guide to Ultrasound-Guided Foam Sclerotherapy
LJVascular2023-10-10T15:34:00-07:00Charting Your Course to Vascular Wellness: A Comprehensive Guide to Ultrasound-Guided Foam Sclerotherapy
Enhancing Vein Health with Ultrasound-Guided Foam Sclerotherapy
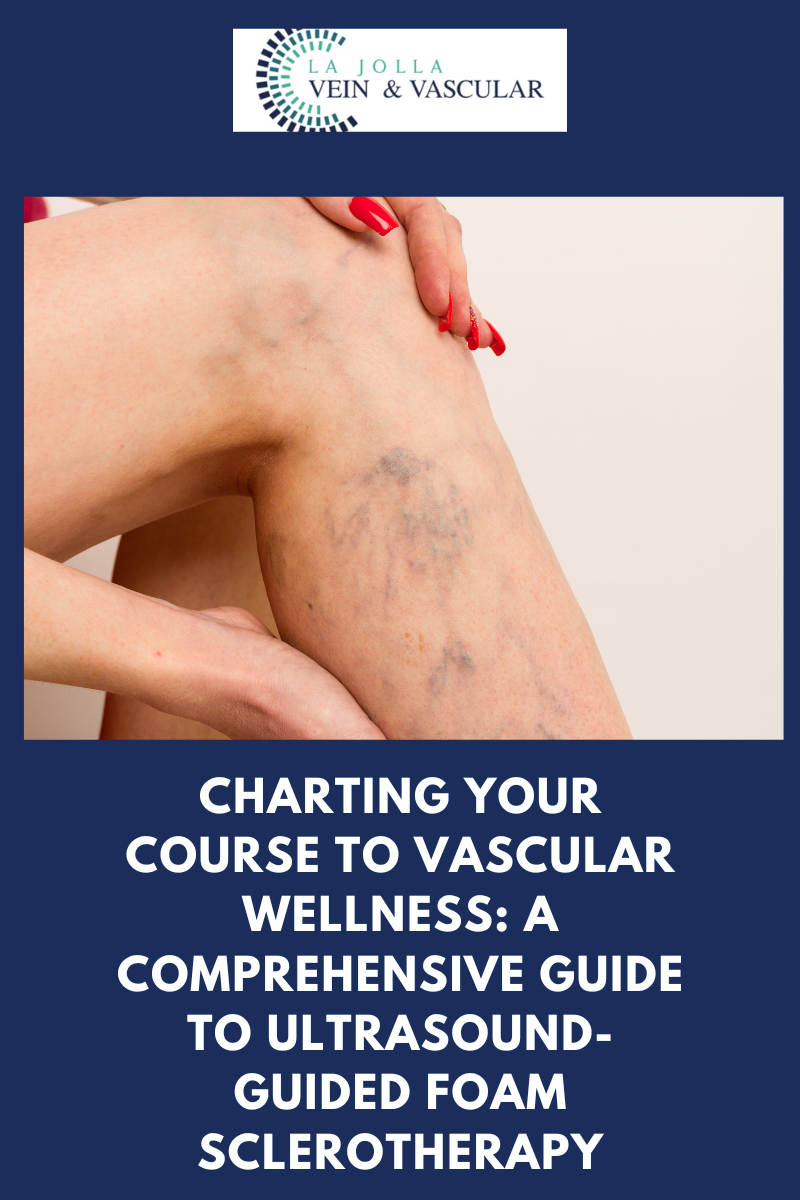
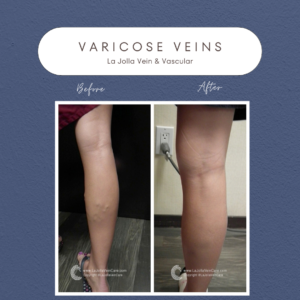
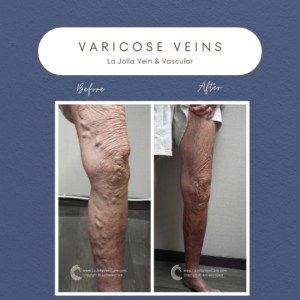
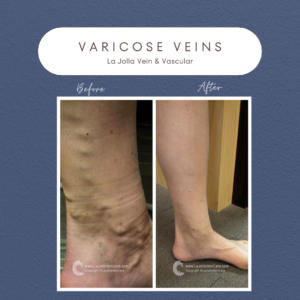
In the battle against visible surface varicose veins and their concealed counterparts, the power of ultrasound-guided foam sclerotherapy takes center stage. This advanced procedure seamlessly marries precision administration with ultrasound visualization, offering a safe and effective solution for a range of vein conditions. In this article, we embark on a deep dive into the world of ultrasound-guided foam sclerotherapy, shedding light on the role of polidocanol (marketed as Asclera®), treatment frequency, and what you can expect during your treatment sessions.
Revealing the Wonders of Ultrasound-Guided Foam Sclerotherapy: A Cutting-Edge Resolution
Ultrasound-guided foam sclerotherapy harnesses the synergy of technology and medical expertise to target varicose veins that may not be readily apparent to the naked eye. The foam medication, skillfully guided by ultrasound, is precisely directed toward varicose veins, even those hidden beneath the surface. This technique is not limited to superficial veins but is adept at navigating complex venous pathways with twists and turns.
Polidocanol (Asclera®): The Preferred Sclerosant
Among the plethora of sclerosant medications, polidocanol, known by the brand name Asclera®, shines as the preferred choice. Its patient-friendly attributes and minimal risk of side effects make it a prime contender for vein treatment. As a detergent-type medication, polidocanol gently disrupts the inner lining of veins, effectively halting blood flow, ultimately leading to complete vein closure. Approved by the FDA for varicose vein treatment since 2010, polidocanol boasts a substantial track record of success in Europe spanning decades. Its transformation into foam for treating larger veins, though an off-label application, has proven remarkably effective and well-tolerated by patients. Rest assured, our seasoned experts at La Jolla Vein Care bring extensive experience to the realm of foam sclerotherapy, ensuring your vein health receives adept and capable care.
Treatment Frequency: A Personalized Approach
The number and frequency of treatment sessions are as unique as your anatomy and individual vein response to treatment. On average, substantial improvement, approximately 80%, can be achieved with 2 to 5 treatment sessions. For some larger or more recalcitrant veins, two or more sessions may be required to achieve a complete response.
Your Treatment Days: An Expertly Guided Sojourn to Vein Wellness
Preparing for your ultrasound-guided foam sclerotherapy treatment day is a streamlined process:
Consent and Attire: You’ll complete a consent form and change into the provided shorts to ensure your comfort.
Skin Preparation: Your skin will be meticulously cleansed with alcohol, and ultrasound will be utilized to pinpoint the veins requiring treatment.
Injection Process: The foam medication will be gently injected into your veins using a fine needle, under the watchful guidance of ultrasound.
Recovery Period: Post-treatment, you’ll elevate your legs using a comfortable wedge pillow for approximately 15 minutes.
Compression Stockings and Walking: After treatment, compression stockings will be thoughtfully applied, and you’ll engage in a 30-minute walk before departing. It’s common to experience some achiness and tenderness following treatment.
Ultrasound-guided foam sclerotherapy ushers in a new era of enhanced vein health, offering precision and efficacy. At La Jolla Vein & Vascular, our dedicated medical team is unwavering in their commitment to delivering personalized care throughout your vein health journey. By embracing cutting-edge techniques such as ultrasound-guided foam sclerotherapy, you embark on a path to healthier, pain-free legs and an elevated sense of well-being.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!