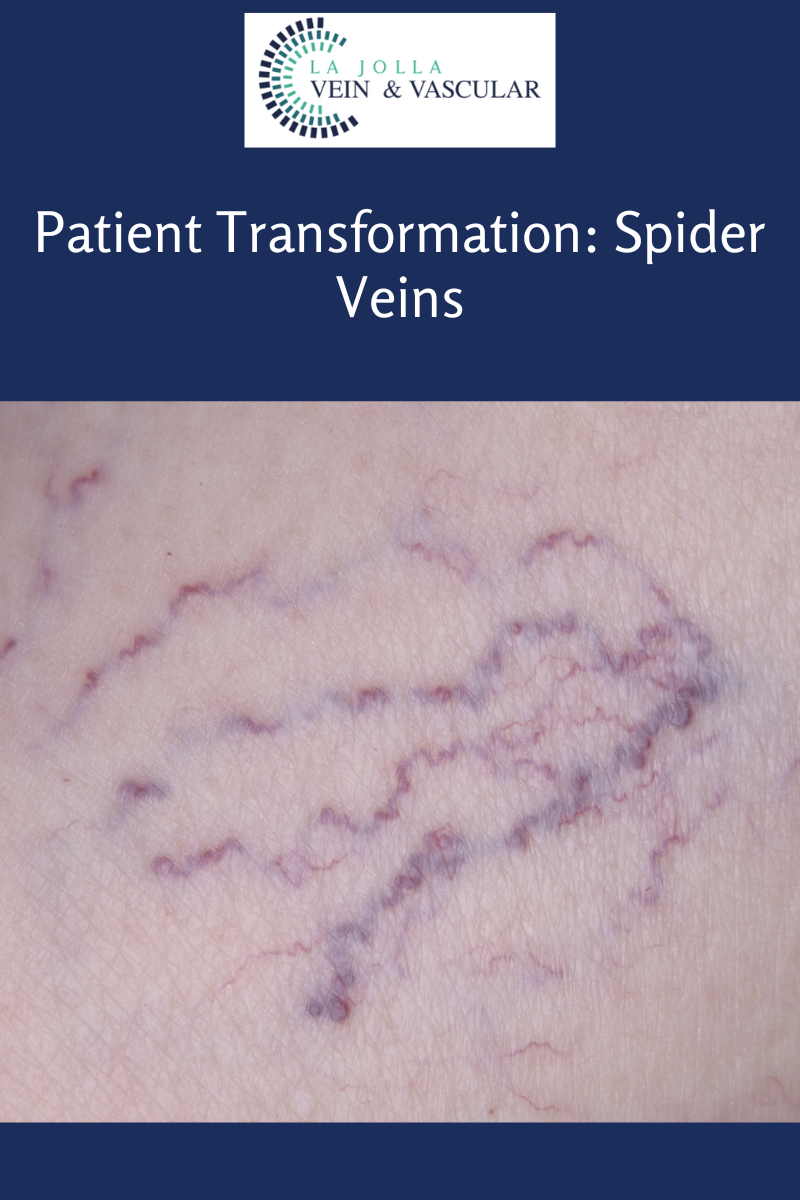
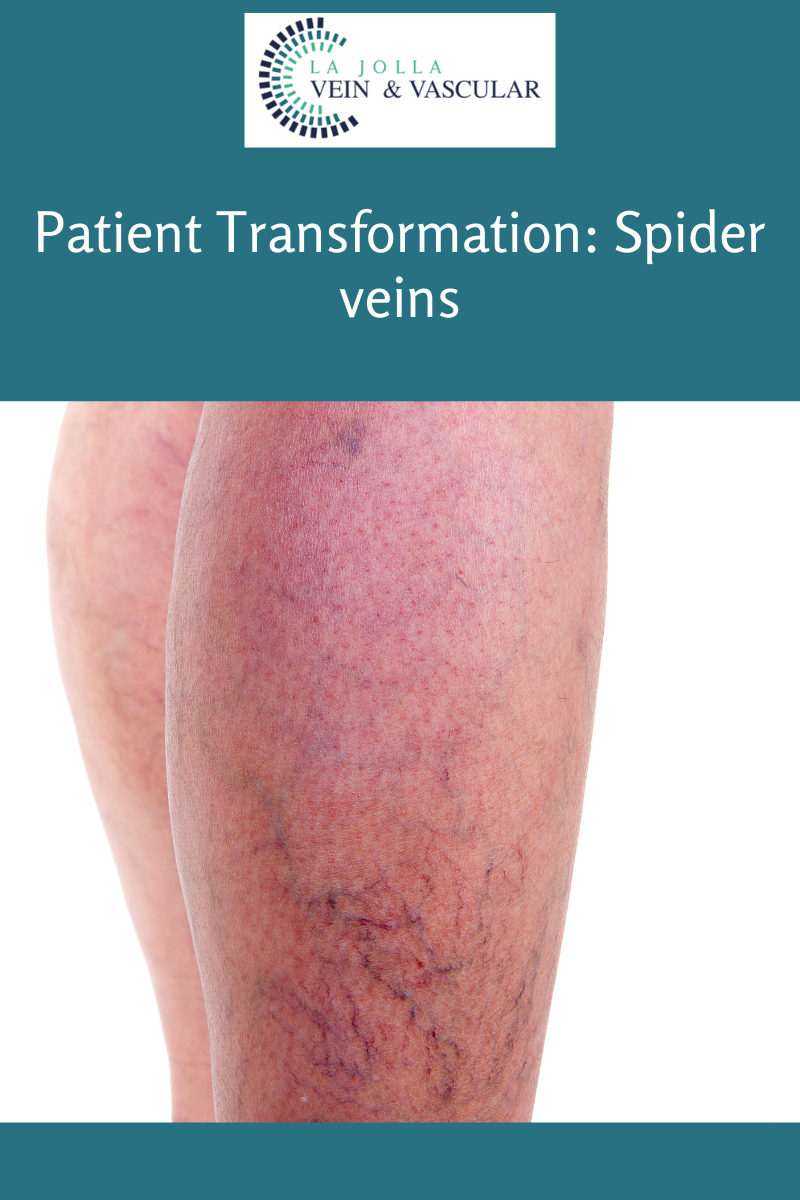
Patient Transformation: Spider Veins
LJVascular2023-02-15T20:42:37-08:00What are spider veins?
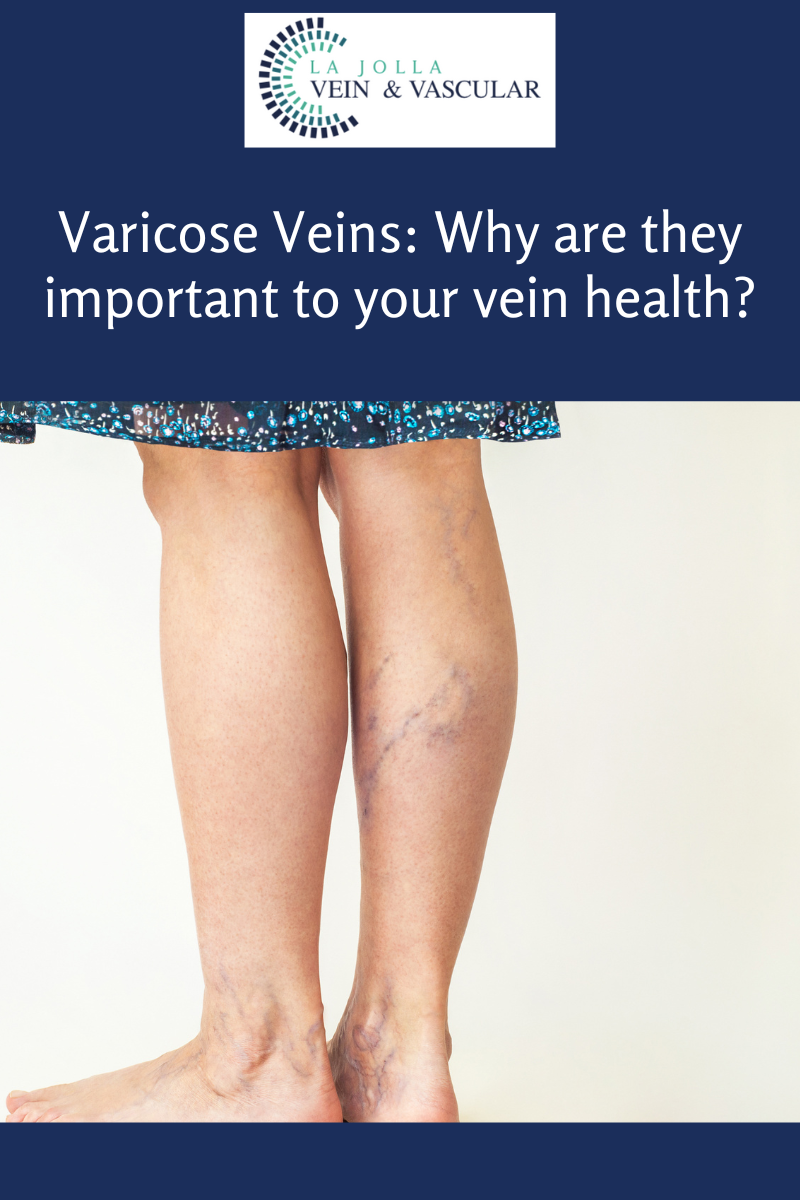
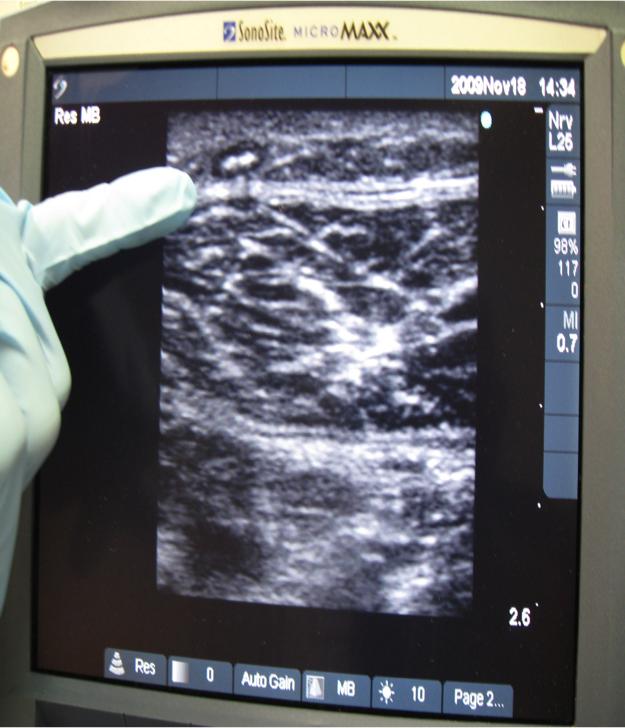
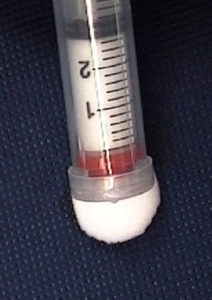
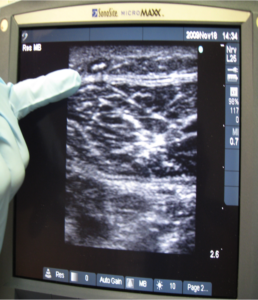
Spider veins are the fine, thread-like reddish veins at the surface of the skin. These veins are not healthy. Veins are often considered a cosmetic issue, but they can be associated with underlying feeder veins, not visible to the naked eye. Feeder veins are the ‘blue veins’ also known as ‘reticular veins,’ that give rise to spider veins. Spider veins may also be a sign of underlying venous insufficiency. For example, spider veins located in the inner ankles and inner thighs can indicate an underlying problem with the saphenous vein. As a result, an ultrasound examination may be recommended to identify and effectively treat the underlying source of these veins.
What are the symptoms?
Vein conditions affect people differently. For some, these veins can be a painless cosmetic concern, and for others they may cause symptoms. The most common symptoms of spider veins are burning, throbbing, and localized pain. They can also feel hot and itchy and bleed.
What causes them?
Spider veins in the legs are caused by the same condition that causes varicose veins. Leaky vein valves allow blood to pool within the veins causing them to stretch and become enlarged. These veins on other areas of the body, such as the face, and chest can be caused by sun damage, hormone changes or liver disease. Hormones, such as with pregnancy, birth control or hormone replacement therapy can weaken the vein wall.
Below you can see the transformation of 3 of our patients who received vein treatment.



“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.