Patient Testimonials Showcasing La Jolla Vein & Vascular’s Impact
LJVascular2023-12-26T16:08:33-08:00Patient Testimonials Showcasing La Jolla Vein & Vascular’s Impact
At La Jolla Vein & Vascular, we take pride in offering holistic care for various vein and vascular conditions. Our dedication to excellence and innovation has resulted in remarkable transformations for our patients. In this blog post, we’ll share the inspiring stories of individuals who experienced life-changing improvements through our advanced vein and vascular treatments.
Understanding Venous Disease
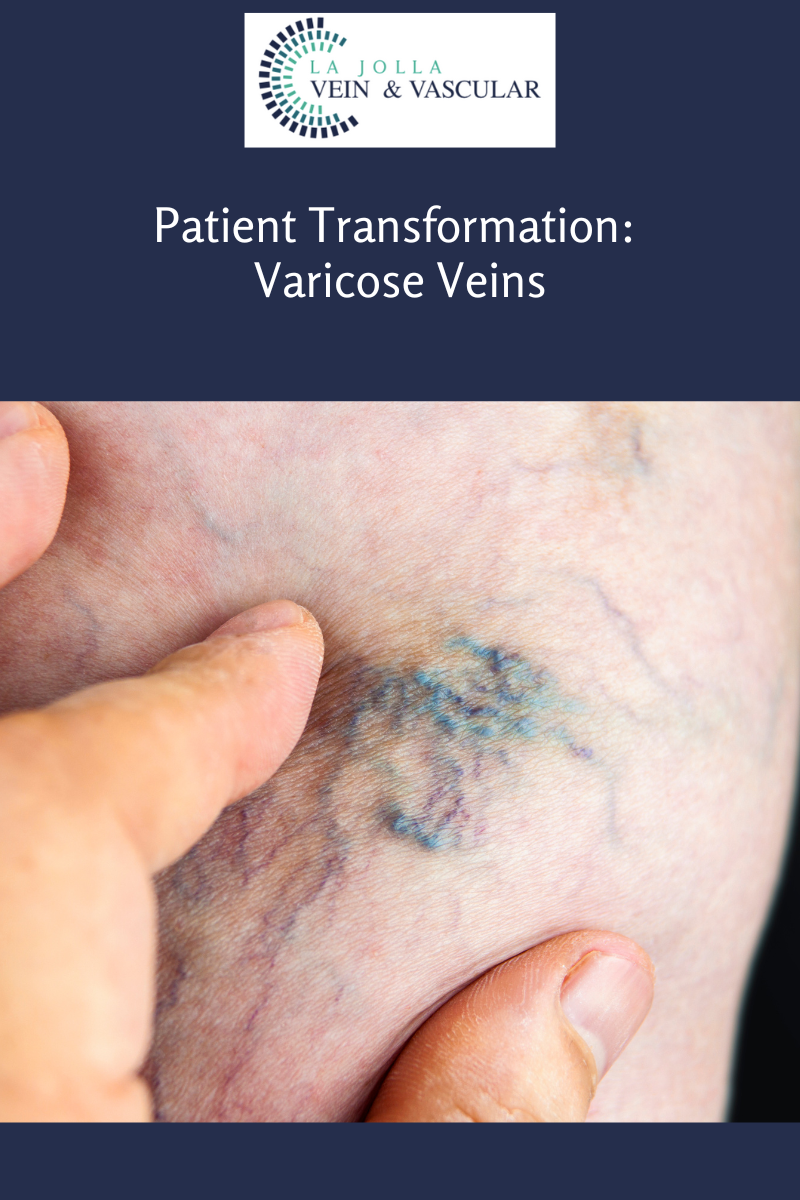
Venous disease encompasses multiple conditions, from spider veins and varicose veins to deep vein thrombosis and chronic venous insufficiency. These conditions can cause discomfort and impact daily life. Recognizing the importance of early intervention, we’ve assembled a skilled team devoted to addressing these issues with tailored treatment plans.
Patient Transformations: Stories of Renewal
Patient 1: Journey to Confidence
A vibrant young woman struggled with spider veins affecting her legs. Feeling self-conscious about wearing her favorite clothes, she sought help at our clinic. Personalized sclerotherapy sessions effectively reduced the appearance of her spider veins, restoring her confidence to embrace her style without hesitation.
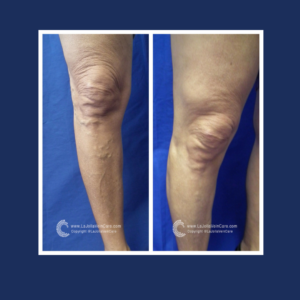
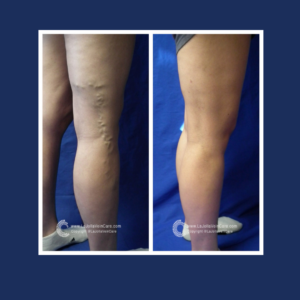
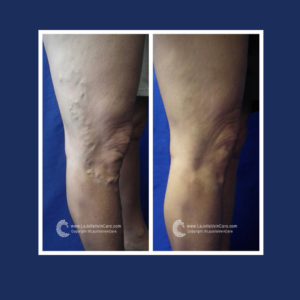
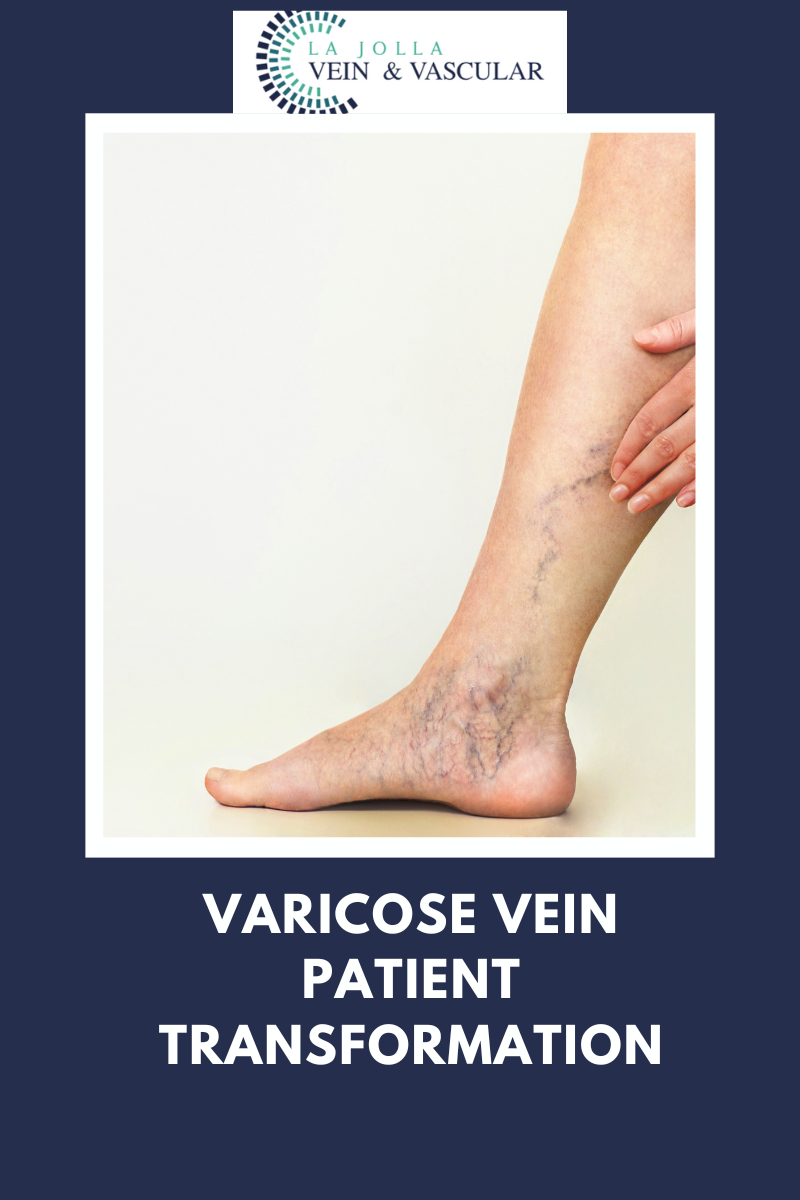
Patient 2: Triumph Over Varicose Veins
An active middle-aged man faced daily disruptions due to throbbing varicose veins. After consulting our experts, he underwent minimally invasive radiofrequency ablation procedures. This not only relieved his discomfort but also allowed him to return to outdoor sports and enjoy quality time with his family.
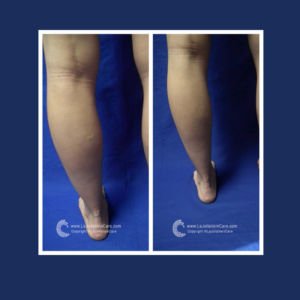
Patient 3: Rediscovering Comfort
A retiree coping with chronic venous insufficiency experienced leg swelling and discomfort that affected her active lifestyle. Through ultrasound-guided foam sclerotherapy and a comprehensive treatment plan, her swelling reduced, improving circulation and allowing her to rediscover the joy of long walks and gardening.
Our Approach to Transformation
At La Jolla Vein & Vascular, our patient-centric approach involves personalized consultations, advanced diagnostics, and tailored treatment plans. We believe in empowering patients with knowledge about their conditions and involving them in decision-making. Our commitment to staying at the forefront of medical advancements ensures that patients receive cutting-edge treatments.
Join Us on the Path to Wellness
If you or a loved one are dealing with vein and vascular conditions, join us on a journey toward improved wellness. Our dedicated team offers effective treatments and compassionate support. Each patient’s story is unique, and we’re committed to being part of your journey to better vein health.
These testimonials illustrate the profound impact of comprehensive vein and vascular treatments. Through innovative procedures and patient-centered care, we aim to bring about positive transformations that extend beyond the physical.


“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!