Why do I have leg pain?
LJVascular2024-03-26T16:03:52-07:00Leg pain can stem from various sources, necessitating the identification of the underlying cause for suitable treatment. In this article, we’ll delve into the diverse factors contributing to leg pain, encompassing vascular issues like poor circulation, varicose veins, and blood clots, along with non-vascular causes such as injuries, arthritis, and low back discomfort. Discover more about the distinct types of leg pain and how seeking professional evaluation can lead to effective relief.
Understanding the Causes of Leg Pain
Vascular Factors:
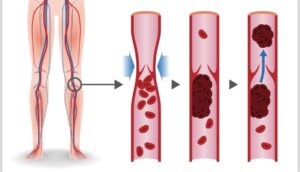
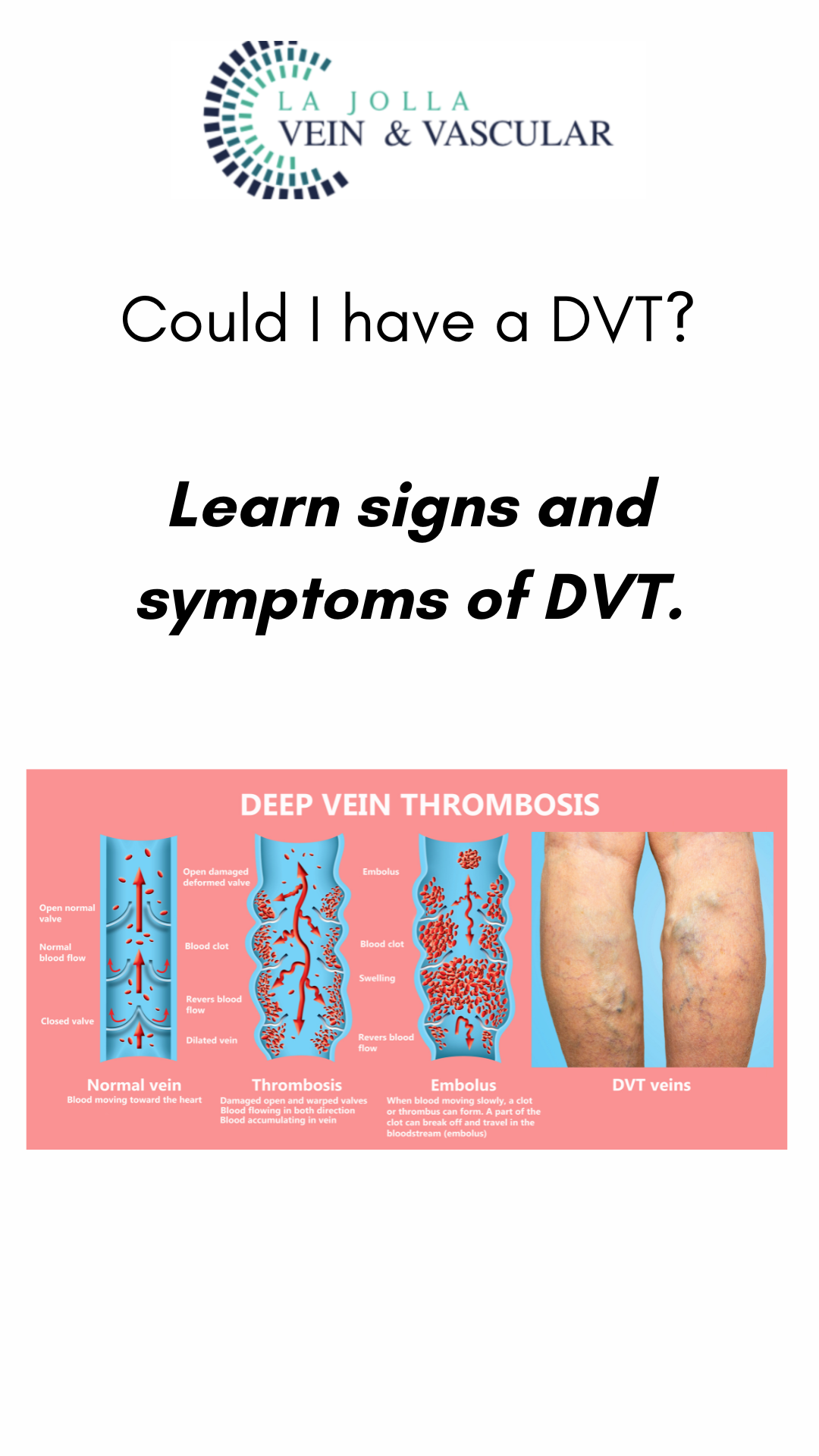
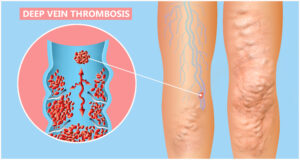
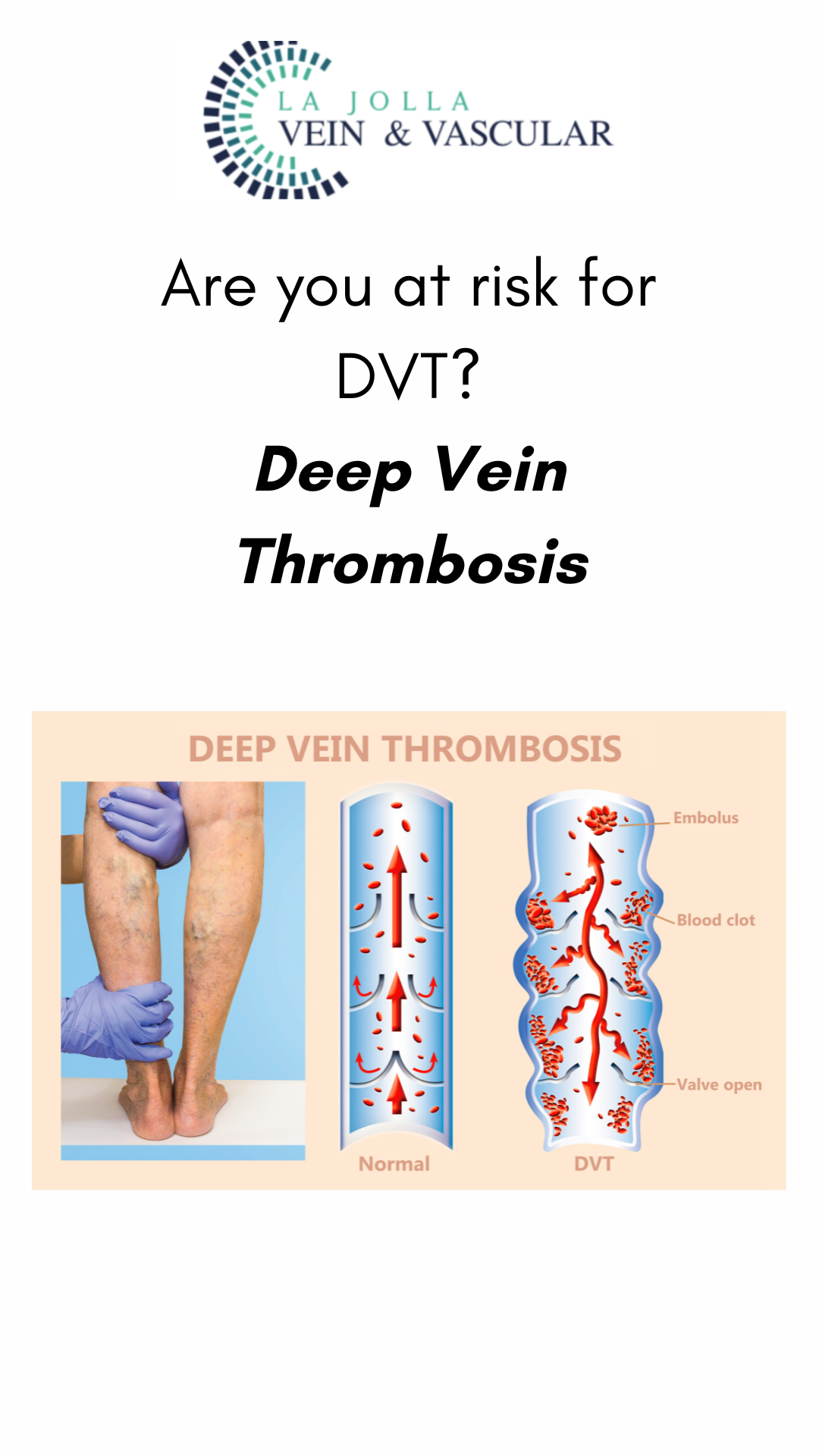
Blood Clots: Whether deep vein thrombosis (DVT) or superficial vein thrombosis, blood clots can induce leg pain. DVT might cause sudden swelling, pain, redness, and warmth in one leg. Superficial vein thrombosis typically affects varicose veins, causing pain, hardness, and a cord-like sensation beneath the skin.
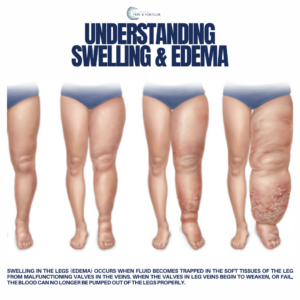
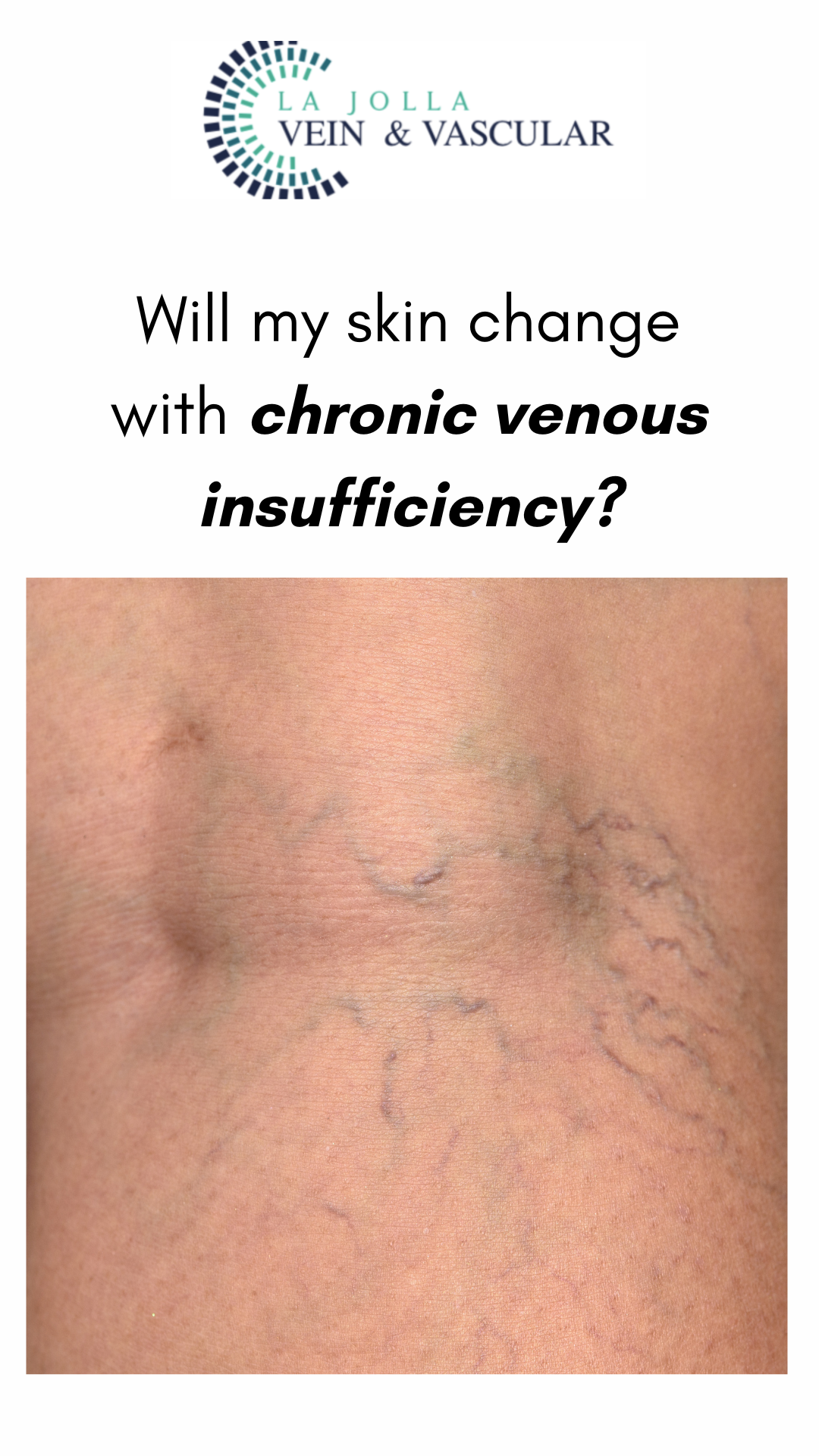
Venous Reflux Disease: Characterized by leg pain, heaviness, and fatigue worsening with prolonged standing, this condition can be exacerbated by hormonal influences in women. Nighttime leg cramping and restlessness are common, often accompanied by visible signs like varicose veins, ankle swelling, and skin changes such as darkening or ulceration.
Non-Vascular Causes:
Injuries: Injuries to joints, bones, muscles, or ligaments can result in localized leg pain.
Arthritis: Arthritic conditions can lead to persistent leg discomfort.
Low Back Pain: Leg pain originating from the lower back can radiate down to the legs.
Understanding Peripheral Arterial Disease (PAD)
Peripheral arterial disease refers to insufficient arterial circulation in the legs, causing leg pain—particularly during walking—and characterized by cramping, especially in the calf muscles. Typically, resting alleviates the discomfort, accompanied by additional signs such as pale toes and absent pulses in the feet.
Diagnosing and Managing Leg Pain
Diagnosing the origin of leg pain involves a comprehensive approach:
Medical History: Healthcare providers gather information about your medical background, symptoms, and any risk factors.
Physical Examination: A thorough exam can unveil signs of vascular or non-vascular issues.
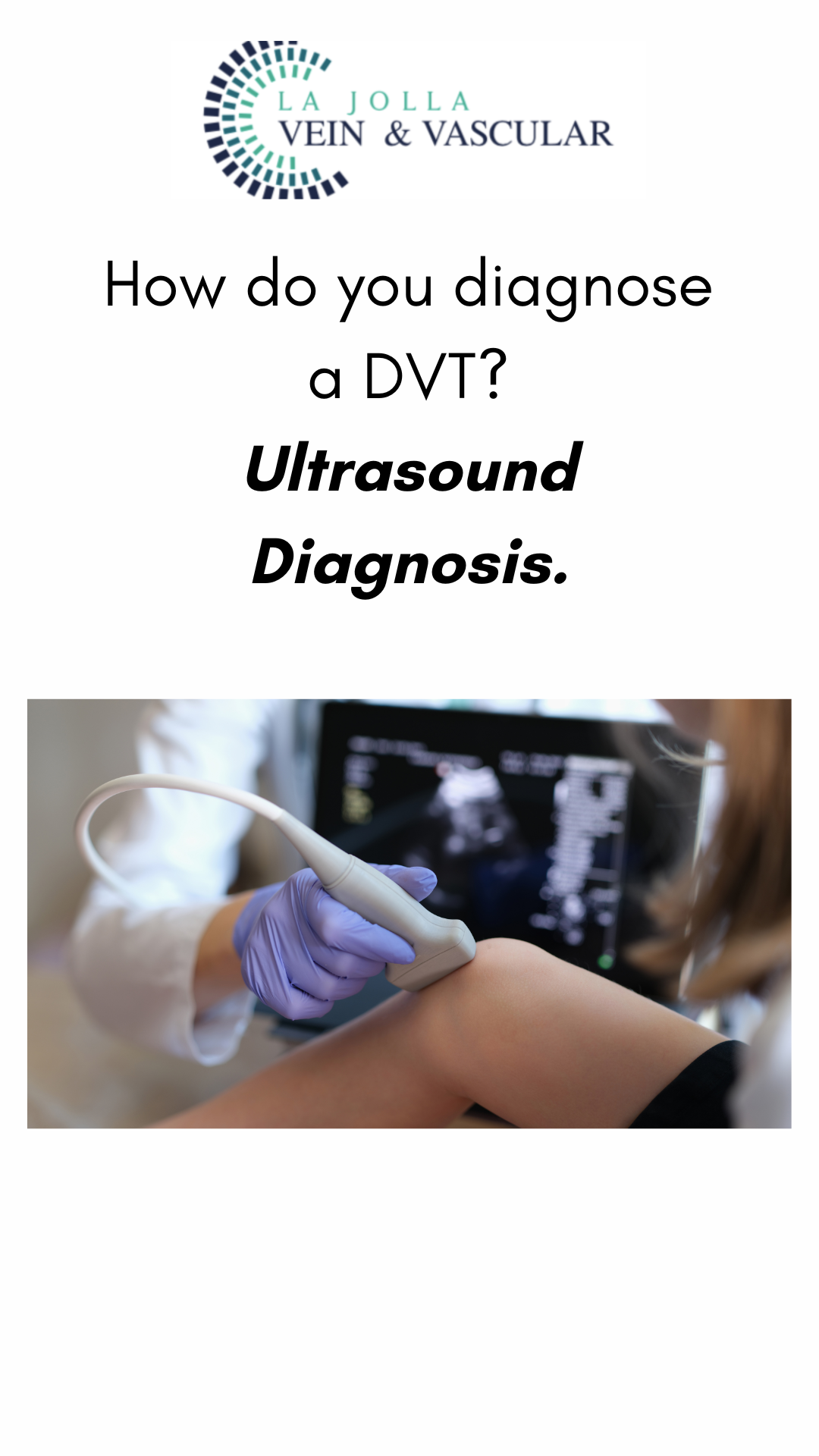
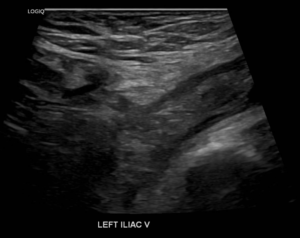
Non-Invasive Ultrasound Imaging: This imaging technique aids in visualizing blood flow and identifying potential vascular problems.
ABI Test: An Ankle-Brachial Index (ABI) test can screen for peripheral arterial disease.
Treatment Options and Relief
The encouraging news is that all these conditions are treatable, often through enhancing blood flow. Once diagnosed, suitable treatment plans, including lifestyle modifications, medications, minimally invasive procedures, and more, can be devised. Seeking professional guidance is crucial for tailoring the right treatment approach specific to your condition.
Seeking Relief for Leg Pain
If you’re grappling with leg pain, seeking professional evaluation is imperative. Understanding the root cause of your discomfort marks the initial step towards finding effective relief. Whether your leg pain originates from vascular or non-vascular sources, remember that viable treatment options exist. By consulting healthcare providers specializing in these conditions, you can restore comfort and mobility. Reach out to us at 858-550-0330 to schedule a diagnostic imaging session and consultation with our dedicated healthcare providers. Your journey towards pain-free legs commences with a simple call.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!