Approach to Vein Treatment
Nisha Bunke2020-09-18T18:51:19-07:00Venous Reflux Disease is Treated By a Staged Approach
Step 1: The Underlying Problem
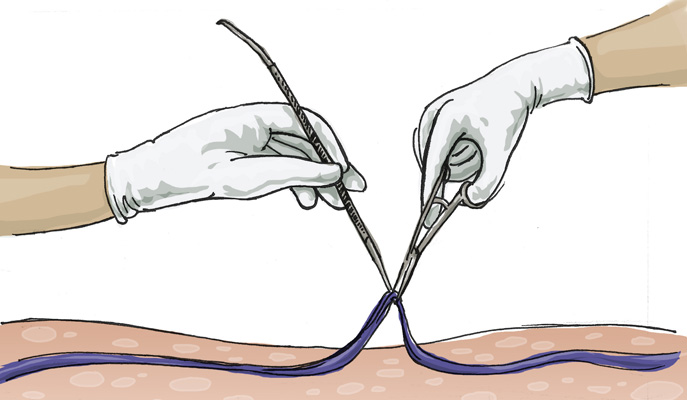
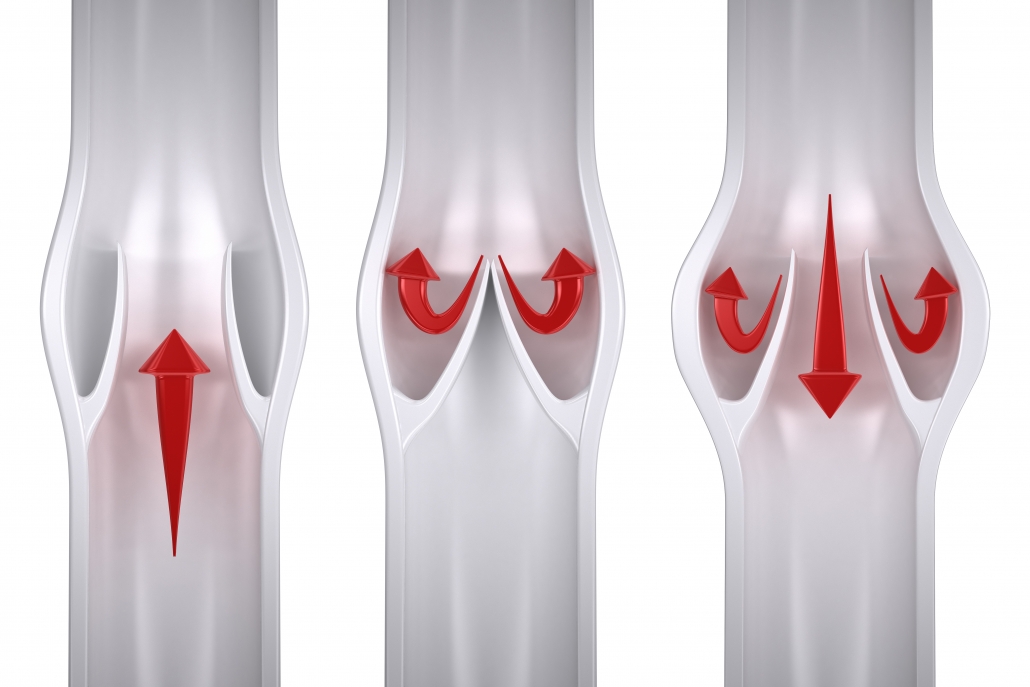
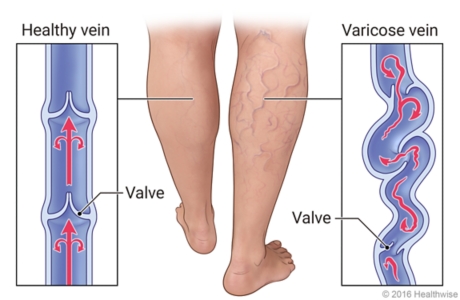
The first step is to treat the underlying problem, the venous reflux. The specific pattern of venous reflux was detected by ultrasound. Venous reflux usually starts in the saphenous veins. The saphenous veins are most effectively treated with vein ablation procedures. This involves placing a small catheter within
the vein and using heat or a solution to produce injury and eventual closure of
the vein. The most commonly used treatments for the saphenous veins are radiofrequency ablation (RFA), laser ablation, mechanico-chemical ablation
(MOCA or Clarivein), and in some cases Varithena Foam. The treatment Step recommendation is customized, based on where reflux is present and other clinical factors.
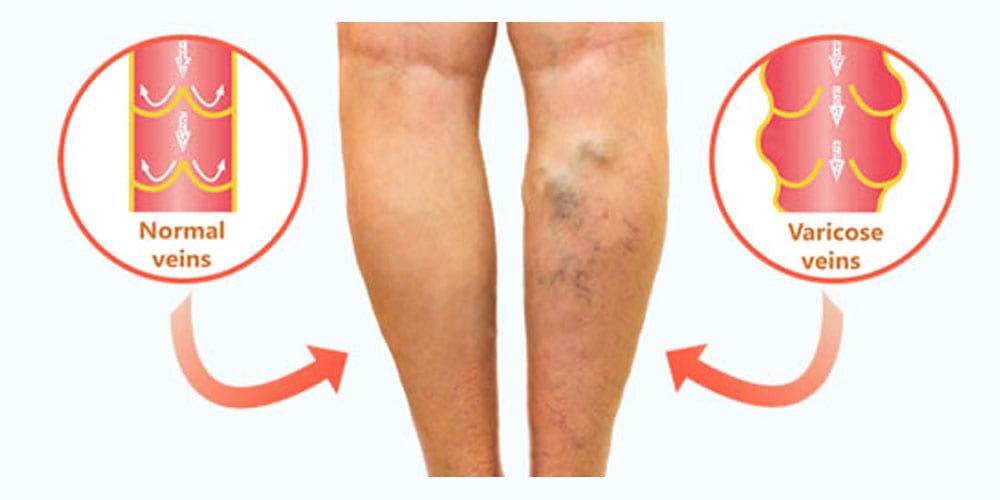
After the underlying saphenous vein reflux is corrected, the bulging veins (varicose veins) can be treated by injecting a foamed medication that will cause them to scar and eventually dissolve (foam sclerotherapy), or to remove them using tiny incisions. The most common method is foam sclerotherapy. This is also known as ultrasound-guided foam sclerotherapy (UGFS).
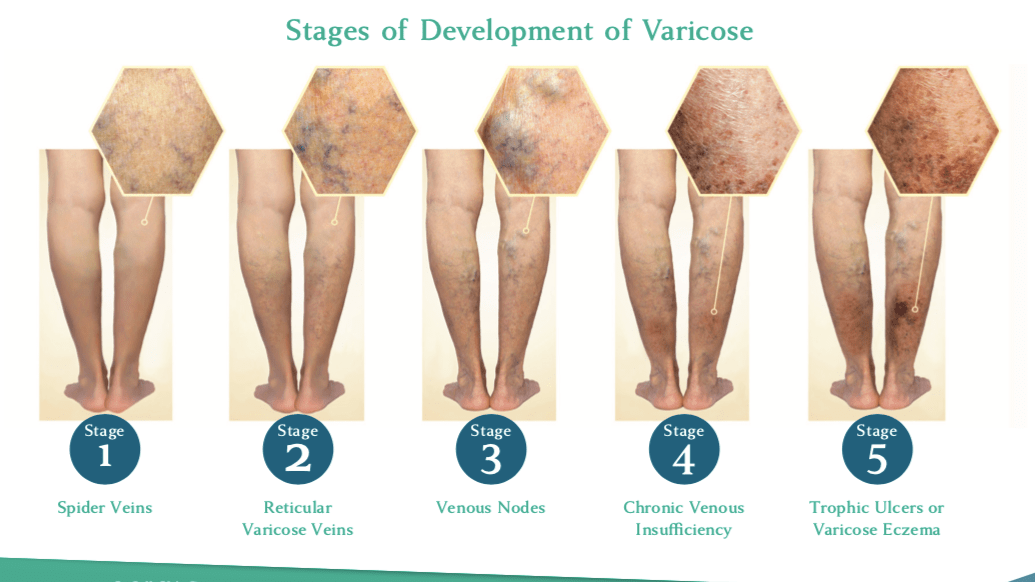
Step 3: Spider Veins
Spider vein treatment is always considered a cosmetic procedure. If improved cosmesis is a goal of treatment, make sure to discuss this with your doctor and plan on having cosmetic treatment as the last step. Spider vein treatment is accomplished by sclerotherapy, which is an injection of a liquid medication into the spider veins. Ask your provider for an estimate about how many treatment sessions/ vials are necessary to get the results you want.