The Best Treatment for Saphenous Vein Reflux
LJVascular2022-03-17T10:11:22-07:00The best treatment for Saphenous Vein Reflux is tailored to the individual
Fortunately, there are a variety of non-surgical treatment options for saphenous vein reflux, the underlying cause for varicose veins and it’s symptoms. Because vein treatment is not, ‘one treatment fits all,’ the treatment plan should be customized to the patient. Non-surgical options include, laser vein ablation, radiofrequency vein ablation, varithena foam, venaseal an mechanical-chemical ablation, also known as clarivein. This article will specifically discuss features about Clarivein which make it a good option for some patients.
Mechanical-Chemical Ablation (Clarivein) for Saphenous Vein Reflux
The ClariVein procedure for treatment of backwards flow (or reflux) in your saphenous veins. The great and small saphenous veins are the two main superficial veins of the leg. They run along the inner leg and the back of the leg. This minimally invasive procedure can be performed in the office in less than an hour. This offers patients the benefit of being able to return to their usual level of activity the same day.
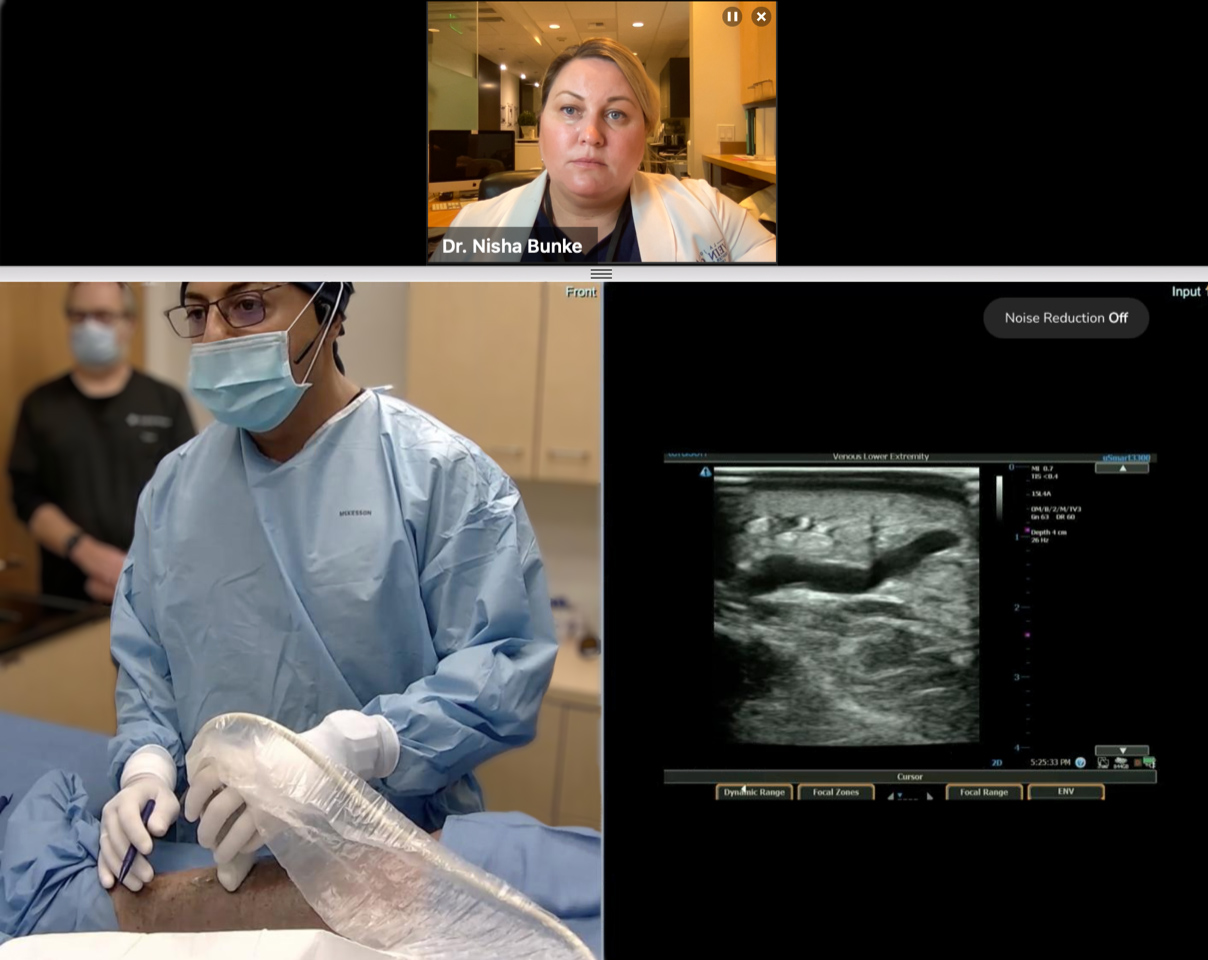
How does the treatment work?
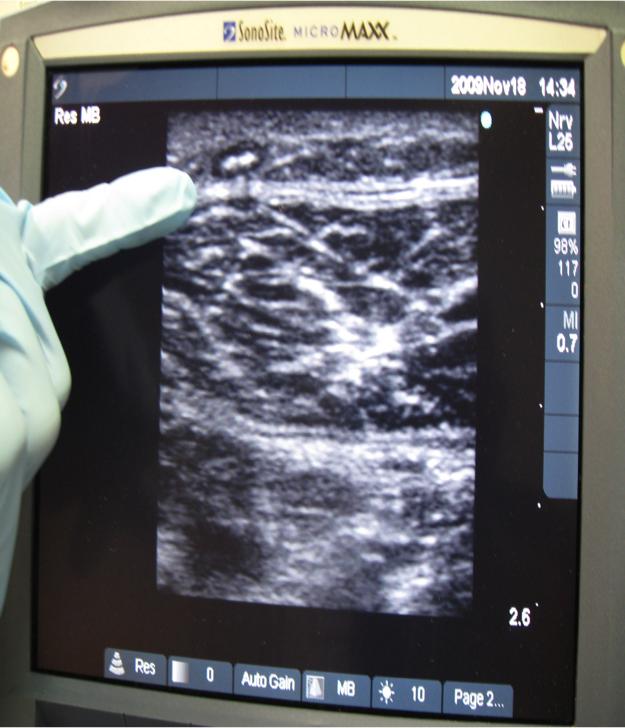
The skin is numbed with lidocaine, then the ClariVein catheter is placed into the unhealthy vein. The catheter closes the vein painlessly by delivering two treatments:
- Mechanical treatment with a tiny rotating wire.
- Chemical treatment with polidocanol.
This technique is highly effective in closing the vein and only requires one skin puncture, similar to placing an iv.
What should I expect on the day of treatment?
The procedure is performed with local anesthesia, but many patients elect to use a mild oral sedative (Valium), which is taken after checking in and completing all paperwork. The patient will change into a gown and leave underwear on. Depending on the vein to be treated, the patient will lay on the back or on the belly. We do our best to make special accommodations (for example, if the patient cannot lie flat or cannot bend a knee very well) with body positioning and using pillows. We will do our best to make the patient comfortable. Then, we will give the option of watching a movie on Netflix or listen to music. Once the patient is comfortable, the leg will be prepped with a cleansing solution for the sterile procedure. The doctor will perform an ultrasound to map the vein to be treated. Then, a numbing agent (lidocaine) will be injected into the skin. In the numb area of the skin, a tiny puncture is made to pass the ClariVein catheter. Once the catheter and rotating wire are in place, the doctor will start the treatment. It is common to feel a tickling or vibrating sensation as the doctor treats the vein. Patients usually have minimal to no pain during this procedure. Once the vein has been treated, the patient will wear compression stockings for 72 hours continuously. The benefits of wearing compression stockings during post surgical recovery are mentioned here.
What should I do after treatment?
You should walk 30 minutes twice daily after treatment and move your legs frequently throughout the day with short walks and/or calf exercises. This will alleviate discomfort and avoid pooling of blood in the legs. It is normal to have aching in the treated veins. This responds well to walking, ice packs, and anti-inflammatory medications such as ibuprofen (Advil, Motrin) and naproxen (Aleve). Compression stockings are recommended for after treatment.
What should I avoid after treatment?
For at least two weeks after treatment, you should avoid strenuous exercise (anything more than a brisk walk), heavy lifting, saunas or hot tubs, and leg massages. All of these dilate the superficial veins and interfere with their healing. You should also avoid airline travel for two weeks after treatment.
What are the possible adverse effects?
Expect some bruising over the puncture site, which fades over about two weeks. The skin overlying larger varicose veins may also develop some temporary inflammation and/or brownish hyperpigmentation as the blood products within those veins are absorbed by the body. An uncommon complication is a blood clot within a deep vein.
Videos of the treatment, as well as after care instructions can be found on our website or our Youtube Channel.