Deep vein thrombosis (DVT) is a condition in which a blood clot forms in the deep veins located in the leg, thigh, or pelvis. While Deep vein thrombosis (DVT) is common in the lower leg, it can also develop in other body parts, including the arms. So, how do blood clots form in the veins, and is it dangerous?
To answer this, let us look at how the blood circulates in the body. The blood circulatory system consists of two blood vessels, namely the arteries and veins. The arteries carry blood rich in nutrients and oxygen from the heart, while the veins carry the deoxygenated blood back to the heart. Arteries have thin muscles within their walls that make them capable of withstanding the pumping pressure from the heart. However, the veins have no muscle lining and entirely depend on the muscle movement to take the blood back to the heart.
How do Blood Clots Form?
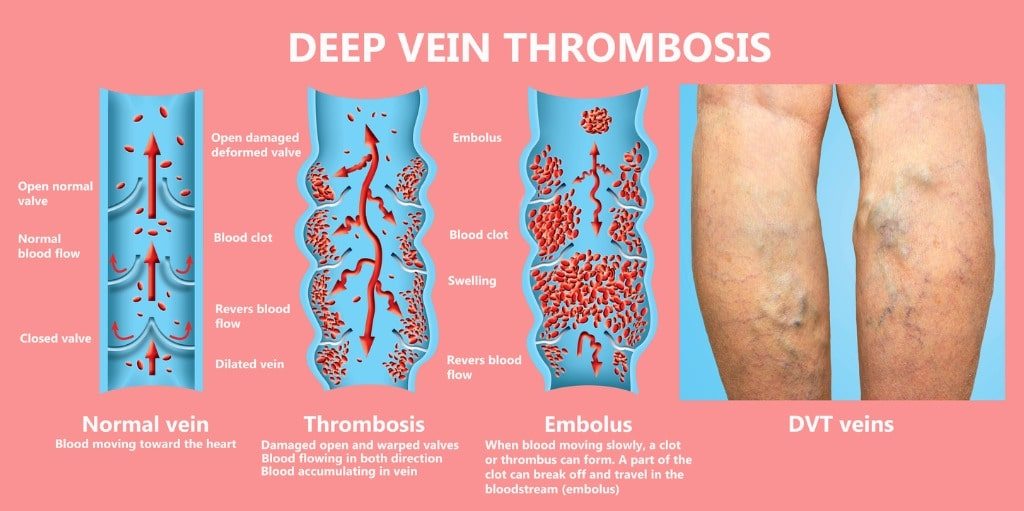
The venous system in the legs consists of two main veins, the superficial veins, and deep veins. As the name suggests, deep veins are located deep within the muscles. On the other hand, superficial veins are located just below the skin and are easily visible. Typically, the blood flows from the superficial veins into the deep venous system through perforator veins. Both the perforator and superficial veins have valves that allow blood to flow in one direction.
However, when blood travels slowly in the veins or pools in the veins, the platelets tend to stick together. While a blood clot (thrombus) in the deep venous system of your leg is not dangerous by itself, it can become life-threatening when it breaks and travels to enter the pulmonary vein. When the blood clot blocks a pulmonary artery, it decreases the amount of oxygen absorbed in the blood, causing a life-threatening condition known as pulmonary embolism.
Deep vein thrombosis (DVT) is considered a medical emergency. According to the CDC (Center for Disease Control and Prevention), 10 – 30 percent of individuals who develop leg DVT experience life-threatening complications within a month of diagnosis.
DVT SYMPTOMS
Like other disorders that affect the venous system, some individuals with DVT may not notice any symptoms. However, if the symptoms develop, people with deep vein thrombosis (DVT) may experience the following:
- Leg pain with walking (muscle cramp or sharp pain)
- Sharp pain in the affected limb that starts in the calf
- Red or discolored skin on the affected limb
- Swelling in the affected limb
- Sudden onset leg swelling
- Enlarged veins
- Increased warmth in the swollen, painful region
Most often, deep vein thrombosis (DVT) affects only one leg, although, on rare occasions, the condition may develop in both legs. If the blood clot (thrombus) breaks and travels up to the lung, a person suffering from pulmonary embolism may have the following:
- Sudden breathlessness or slow breathing
- Rapid breath
- Increased heart rate
- Chest pain that worsens when breathing deeply
At La Jolla Vein & Vascular
We Treat Deep Vein Thrombosis (DVT)
DVT treatment options include:
• Blood thinners. DVT is most commonly treated with anticoagulants, also called blood thinners. These drugs don’t break up existing blood clots, but they can prevent clots from getting bigger, prevent the clot from breaking loose and traveling to the lungs and reduce your risk of developing more clots.
Blood thinners may be taken by mouth or given by IV or an injection under the skin. The most commonly used injectable blood thinners for DVT are enoxaparin (Lovenox) and fondaparinux (Arixtra). Oral medications such as Eliquis, Xarelto and Pradaxa are well tolerated and are more common than injections in the out-patient setting. Sometimes warfarin is used, but less commonly as it requires regular blood tests and monitoring
Oral medications can be started immediately after diagnosis.
Pregnant women shouldn’t take certain blood-thinning medications like most oral blood thinners, but can usually take lovenox injections safely. Collaboration with you OB doctor is important to choose a medication safe for mom and baby.
You might need to take blood thinner pills for three months or longer. The time frame depends on the cause of the clot, the extent and severity and risk for another clot in the future. If an underlying blood clotting disorder is suspected, you may be referred to hematology for blood tests and long term recommendations.
• Clot busters. Also called thrombolytics, these drugs might be prescribed if you have a more serious type of DVT or PE, or if other medications aren’t working.
These drugs are given either by IV or through a tube (catheter) placed directly into the clot. Clot busters can cause serious bleeding, so they’re usually only used for people with severe blood clots.
• Filters. If you can’t take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs.
• Compression stockings. These special knee socks reduce the chances that your blood will pool and clot. To help prevent swelling associated with deep vein thrombosis, wear them on your legs from your feet to about the level of your knees. You should wear these stockings during the day for at least two years, if possible.
OUR PATIENTS SAY

We were early and didn’t have to wait at all. The tech that did my husband’s ultrasound, Monica, was very accommodating with my husband’s Parkinson’s. Doctor Lucas whom we hadn’t seen before, came to us instead of making my husband walk down to another office. She spent a lot of time getting caught up on Steve’s background issues/conditions. I was impressed by this medical group before, so I was surprised that the staff was even better this time around; I honestly didn’t think there was room for improvement!
The office is exceptional, from front desk, to exam staff to the physicians. They have created a welcoming, relaxing environment, and take their time in examining and consulting with you to provide the best outcome. I highly recommend La Jolla Vein & Vascular for the assessment and treatment of your vein and vascular function.
When I arrived for the first time, I could barely walk. My legs were red and swollen. After my treatments, I can now walk again. I’m so thankful to the doctor and his staff. They are caring, supporting and knowledgeable about my issues. Five Stars all the way!!!!
Beautiful facility! I walked in without an appointment and they took me right away! It was even the end of the day…I was so grateful…Every single person was soooo pleasant! Super impressed ❤️
The staff members that I interacted with were all professional, conscientious and empathetic to my complaints and discomfort. I was taken into the ultrasound room a few minutes before my appointment time. I did not have a long wait before the ultrasonographer came and ran the machine. It was also a short wait before Dr. Steinburg came into the room with a warm, welcoming smile. We discussed my ultrasound and the things I was experiencing . I scheduled another appointment for next year and was offered a bottle of water upon leaving the office. All in all, I thought it was a very satisfactory appointment.
The staff kept you informed as to when you would be seen and the wait was not too long. Emily took care of my ultrasound and was very accommodating giving me an extra pillow and playing a video to watch. The office is very courteous and professional- Nadia answered our questions and offered us a bottle of water. I have been seeing Dr. Bunke, but now Dr. Lucas and will continue coming to La Jolla Vein Care!
From my greeting at the front desk to the ultrasound and visit with the doctor, I received excellent care. It’s clear they care about their patients and all the staff couldn’t have been nicer or more helpful. I also appreciate how much time the doctor spent with me to explain the results and the next steps. I would definitely recommend this office to friends with vein issues.
La Jolla Vein care has the best staff ever. They are so nice, accommodating and professional!! Dr. Bunke is the best doctor that I ever seen. She is so friendly upfront and has the best bed side manner. I thank this office for letting me be their patient. 💜. Plus they are so careful with COVID which I really appreciate!!!
Dr De Young is personable and thorough in his explanations. Exceptional.
Everyone here is so nice! Usually front desk medical personnel are so rude. The front desk ladies Alejandra, Anna, and I think her name is Liz, went above and beyond to take care of me and my insurance issues. The techs are great too! Rachel and a male technician assisted me…both of them implemented different techniques to make me feel more at ease during an uncomfortable and painful process. These procedures were rough…and I am grateful everyone was so sweet to me. Thanks again.
Highly recommend! Entire staff are warm& friendly, professional and accommodating. The doctor took the time to thoroughly explain everything and encouraged me to ask questions. I never felt rushed. Significantly better experience than the other 2 vein clinics I’ve been to on the east coast. I wish I could’ve just come here from the beginning.
The staff at La Jolla Vein Care Center are outstanding. They are friendly and helpful. Dr. Lucas and my ultrasound tech were both very thorough, kind and answered all of my questions. The new office was beautiful. I feel very confident that I am in good hands and that any up coming treatments will be successful. Thank for for making me feel so comfortable.
I have been having leg treatments for several months now La Jolla Vein Care. Every time I go to an appointment; the staff is so friendly and takes such good care of me; always informative; not in a rush and always friendly (especially Alejandra & Anna to name a few). Of course Dr. Lucas is amazing. The treatments have changed my life. Overall this has been an incredible experience.
I had the best experience at La Jolla Vein Care. Dr.Bunke is an amazing doctor with the best bedside manners, she truly cares about her patients, she explained everything to me. My procedures where so easy I was impressed how painless and fast my appointments. Anna M was very helpful scheduling my treatments and checking on me to make sure all of my questions were answered. I am very pleased thank you !!! I truly recommend La Jolla Vein Care!
I am pleased to recommend La Jolla Vein & Vascular. I am in the process of receiving treatment there. The entire medical staff are super friendly, welcoming and very helpful. Everyone is courteous, including the physicians. I’ve had one doctor follow my case. He’s the one who always treats me at appointments and closely follows my health. I am very comfortable going there. Would go again if needed and encourage anyone who’s thinking of making an appointment to do so asap. You’ll see what a wonderful experience it is. It’s the people who make it so special!
Make An Appointment
To make an appointment or to inquire about how we can help you understand your treatment options
La Jolla – Text us or Call 858-550-0330
Vista – Text us or Call 760-249-7007



























