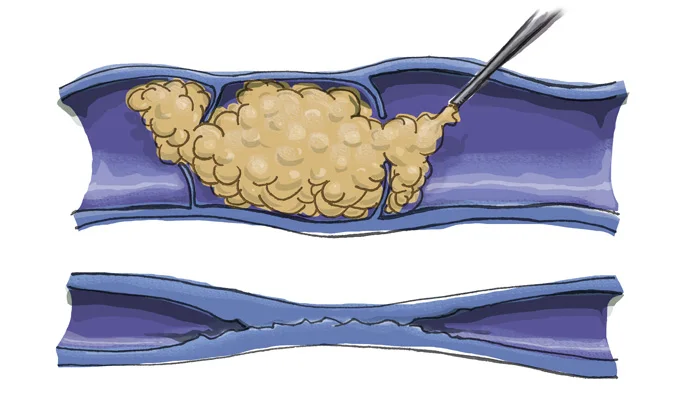
Although treatment cannot reverse existing skin changes in CVI, it can forestall further degradation and ulceration. Addressing the underlying venous reflux diminishes inflammatory changes, potentially alleviating itchiness and dryness. Yet, persistent skin discoloration might endure despite successful reflux treatment. Central to treatment is rectifying the underlying venous reflux.
Venous leg ulcers, a potential outcome of severe CVI, demand a comprehensive healing approach. Treatments may involve:
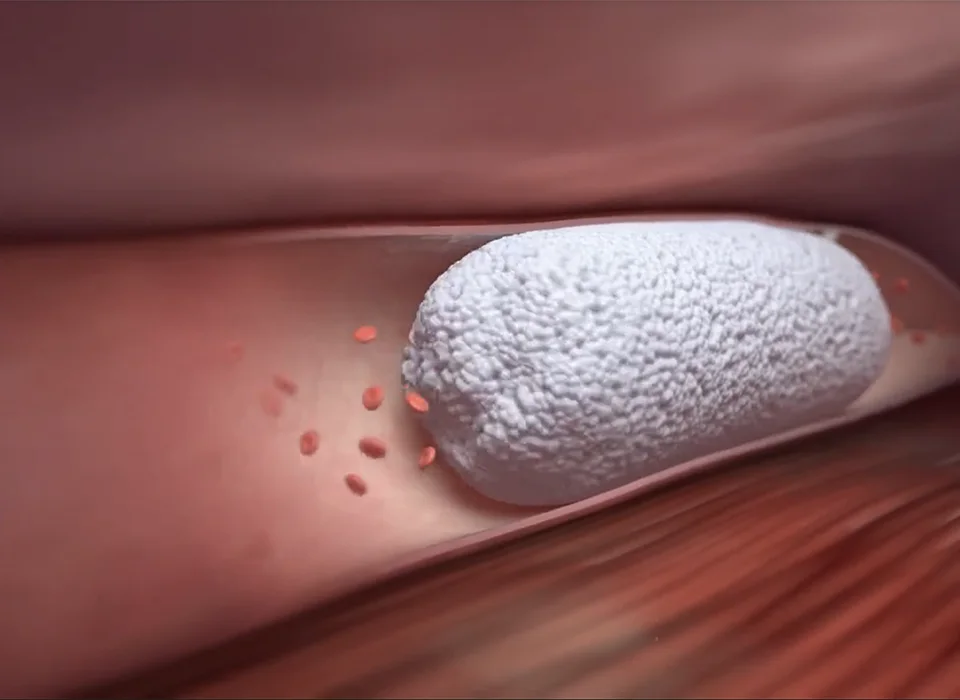
A comprehensive ultrasound examination determines the precise location of the underlying reflux, whether in the saphenous veins, perforator veins, tributaries, or deep veins, guiding the appropriate treatment trajectory.
Chronic Venous Insufficiency entails complex implications for those affected. Armed with understanding the condition, its symptoms, and available treatments, individuals can make informed health decisions, navigating the path to wellness.
Non-healing ulcers fall into distinct categories, each stemming from different underlying factors. The three major classifications are:
The risk factors contributing to non-healing ulcers are diverse but share the ability to disrupt the body’s wound healing mechanisms. These factors include:



 Find out more about SkinPen®
Find out more about SkinPen®
 Find out more about our Laser Treatments
Find out more about our Laser Treatments