Exploring beyond: unraveling lesser known vascular conditions & their impact
LJVascular2023-08-30T18:56:53-07:00Exploring beyond: unraveling lesser known vascular conditions & their impact
At our practice, our dedicated physicians possess specialized training in diagnosing and treating vascular diseases. With a focus on vascular conditions impacting the legs, feet, and pelvis, our experts are equipped to handle a range of issues, from peripheral arterial disease to venous insufficiency and varicose veins. While peripheral arterial disease and venous insufficiency are common culprits, our vascular specialists are well-versed in addressing conditions that require unique expertise, such as varicoceles, Pelvic Congestion Syndrome, May-Thurner Syndrome, geniculate artery embolization, and uterine fibroids.
In collaboration with authoritative sources, such as MedlinePlus.com, we bring you comprehensive information on vascular diseases and their management.
Understanding Vascular Diseases
The vascular system, composed of arteries, veins, and capillaries, forms a network responsible for carrying oxygen-rich blood to tissues and organs while facilitating waste removal. These diseases encompass a spectrum of conditions that affect this intricate system. Our focus lies on several types, including:
- Aneurysm: Abnormal bulging in an artery’s wall
- Atherosclerosis: Plaque buildup within arteries, involving fat, cholesterol, calcium, and other substances
- Blood clots, including deep vein thrombosis
- Varicose veins: Swollen, twisted veins visible beneath the skin
Identifying the Causes and Risk Factors
The origins of vascular diseases vary, with factors like genetics, heart diseases, infection, injury, and certain medications contributing. Risk factors can be diverse:
- Age, often linked to increased risk of certain diseases
- Conditions affecting the heart and blood vessels, such as diabetes or high cholesterol
- Family history of vascular or heart diseases
- Infection or injury damaging veins
- Lack of exercise
- Obesity
- Pregnancy
- Prolonged sitting or standing
- Smoking
Symptoms, Diagnosis, and Treatment
The symptoms of vascular diseases are diverse, depending on the specific condition. Diagnosis involves a comprehensive evaluation, including physical exams, medical history inquiries, imaging tests, and blood tests. Our physicians tailor treatments to the severity and type of vascular disease:
- Lifestyle changes, like adopting a heart-healthy diet and exercising regularly
- Medications, including blood pressure regulators, blood thinners, cholesterol-lowering drugs, and clot-dissolving medications
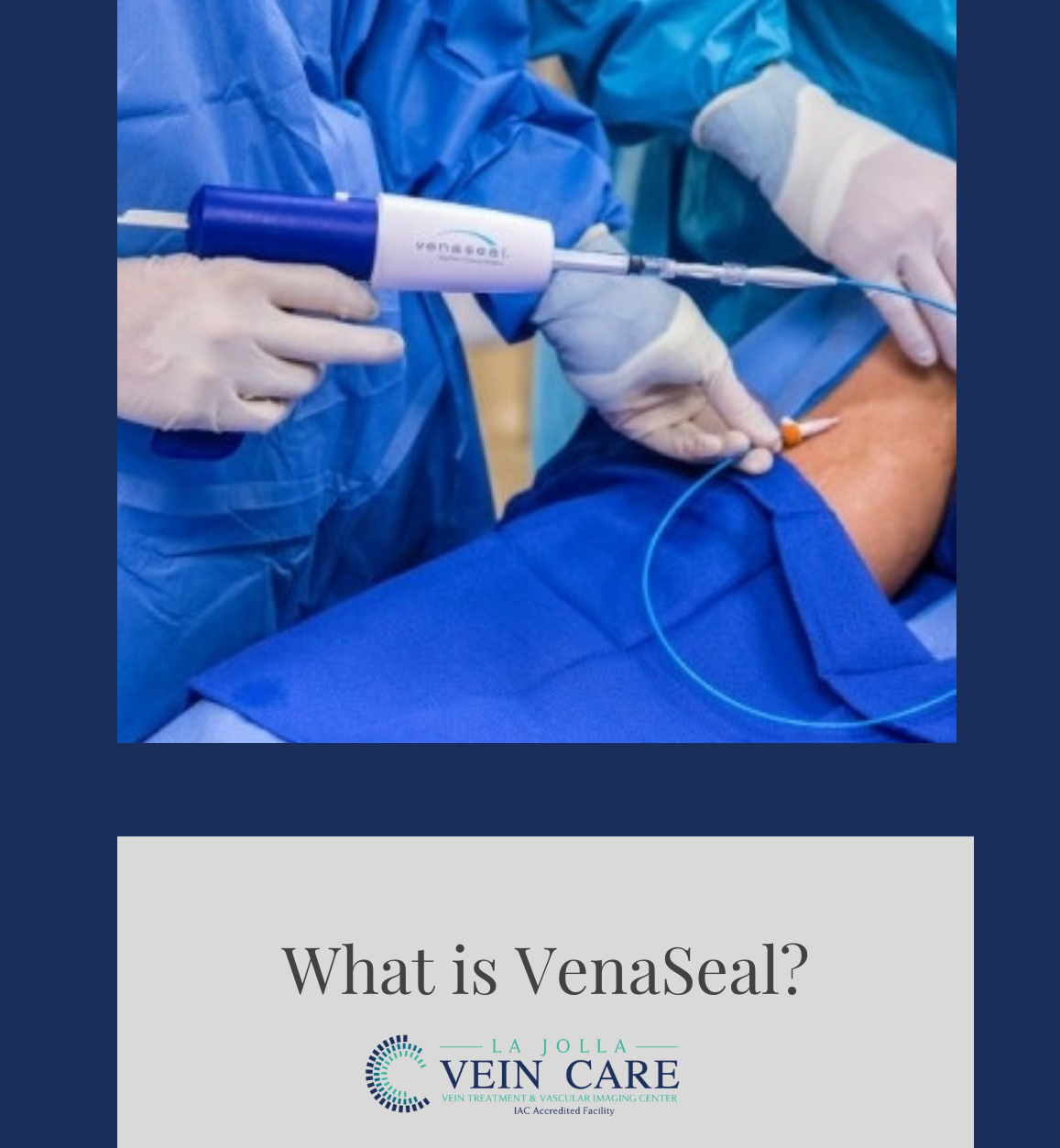
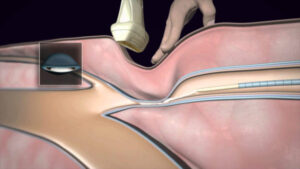
- Non-surgical interventions, such as angioplasty, stenting, and vein ablation
- Surgical procedures
Prevention of Vascular Diseases

Preventing diseases involves proactive steps:
- Embrace a healthy lifestyle through diet and exercise
- Quit smoking or seek professional assistance to quit
- Maintain optimal blood pressure and cholesterol levels
- If you have diabetes, manage blood sugar levels
- Avoid prolonged periods of sitting or standing; move around regularly and consider compression stockings during long trips

Vascular diseases can impact various aspects of your health, but with expert care and proactive steps, you can manage your condition and reduce associated risks. Our specialized team is dedicated to diagnosing, treating, and preventing vascular diseases, ensuring that you receive the highest quality care tailored to your individual needs.
Collaborating with sources like MedlinePlus.com, we aim to provide you with accurate information and effective solutions to enhance your vascular health.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!