Treatment of Non-Healing Wounds & Ulcers
As we’ve seen, there is a very wide range of causes that may contribute to the formation and persistence of non-healing ulcers and wounds. It follows that the methods or treatment options at the disposal of healthcare professionals will also be varied. Doctors will discuss the available options with their patients in order to arrive at the best possible options, but the type and severity of the wound will be the decisive point of consideration. These measures include:
This involves the application of tightly bound wraps to the affected limbs or regions in order to provide support to the vascular system, which might be operating under lower pressure than it should due to the wearing out of the vascular walls and muscles that support the efficient flow of blood to and fro the tissues that need it.
The doctor will start by doing a thorough physical examination. The doctor will also want to learn about your signs, symptoms, personal health history, risk factors, and family health history. The doctor will ask you several questions regarding your medical conditions, such as diabetes, heart disease, and kidney disease. They will also ask you whether you experience pain or cramps in your leg while walking or exercising.
The doctor will also ask about your family history of PAD and other heart diseases. You will also discuss your smoking habit, either current or in the past. After gathering the information, the doctor will proceed to perform a detailed physical examination. The process involves checking for weak pulses in your leg, listening for poor blood flow in the legs using a stethoscope. The physician will also check for any problems on your legs, such as sores, swelling, and pale skin.
Technological progress has made it possible to develop special dressing materials made out of smart polymers that work by adjusting their absorptive qualities depending on the hydration levels of the wound area, among other specialized positive actions. Antibiotics may also be employed topically to non-healing ulcers and these help by reducing the bacterial levels present in the wounds in question while maintaining the optimal levels of environmental moisture suitable for wound repair.
ose PAD. This test usually compares the blood pressure in your arm with the blood pressure in your ankle. The doctor usually uses a pressure cuff together with an ultrasound device. Sometimes, the physician may request you to walk on a treadmill and have the doctor take the readings before and immediately after the exercise. The procedure will help the doctor to capture the severity of the narrowed arteries.
There are plenty of measures that patients will be able to implement in the treatment and management of non-healing ulcers if armed with the proper knowledge and aids where required. Regular cleaning and disinfecting of wounds, proper bandage care, manual repositioning of paralyzed limbs, and avoidance of habits that contribute to the incidence or severity of these types of ulcers will be of significant benefit to many.
This treatment method works by pulling away the fluid in the wound that nourishes bacteria by the application of negative pressure. It is also known as vacuum-assisted wound closure for this reason. This action will also reduce tissue swelling and bring up fresh blood and nutrients to the problem area, which assist in the healing processes.
In many cases, surgical procedures may be called for to rectify any underlying conditions that might be remedied in this way. Patients with atherosclerosis or blood clots in their vascular system, for example, might undergo surgical procedures to remove these clots or clear built-up cholesterol plaques in their system, thus removing the condition that encourages the formation and persistence of non-healing ulcers.
Growth factors refer to the biomaterials generated naturally in our bodies that play the role of replacing tissues as they are damaged or degraded, as in the case of wounds and infections. These factors include epidermal growth factor, insulin-like growth factor (IGF), vascular endothelial growth factor (VEGF), and more. What your medical practitioner will do is introduce or stimulate these factors directly onto the wound in order to speed up the healing and re-growing processes.
Skin Graft Therapy
Skin grafts taken from donors (cadaver, usually) are another option here referred to as allografts. These grafts provide a covering to the wound without integrating with the host body and work by encouraging and providing a structure for the growth of epithelial cells. Severe cases might not be suitable for this intervention, however, and will do better with grafts taken from elsewhere on the patient’s own body.
Debridement more simply refers to the removal of dead or dying (necrotic) tissue from the site of a non-healing wound. The goal is to minimize the risk or opportunity for infection by eliminating the necessary medium for bacterial growth and proliferation, which such tissue provides. This is an especially relevant measure undertaken in the fight against diabetic non-healing ulcers, as amputation will usually be carried out in cases where infection has progressed past a certain limit.
This is the idea behind the rather outlandish yet scientifically sound application of maggot therapy in the management and treatment of chronic wounds. Here, live, disinfected maggots will be introduced to the wound by a medical professional. Maggots will happily devour necrotic tissue while not touching healthy tissue. This directly leads to a reduction in the bacterial presence in the wound, thus encouraging rapid healing as well as pain and odor mitigation.
La Jolla Vein & Vascular Treatments for Non-Healing Ulcers
The treatment for PAD has two main goals. One is to manage the symptoms, including leg pain, allowing you to resume your normal physical activities. The second one is to top the progression of atherosclerosis in the body
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information and to book a consultation, please give our office a call at 858-550-0330.
For more information please check out our Youtube Channel at this link.
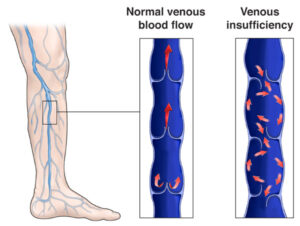
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.