Spider veins causes, risks, symptoms
LJVascular2023-05-25T16:29:19-07:00What are they?
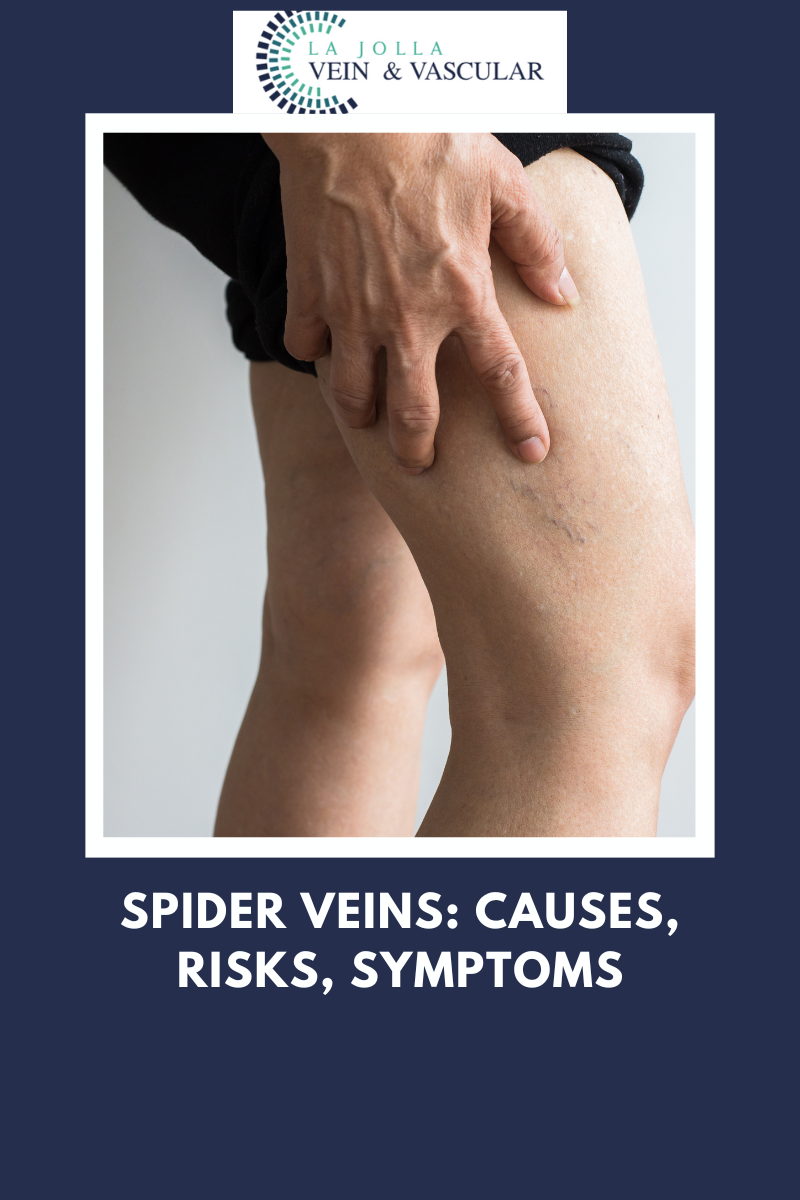
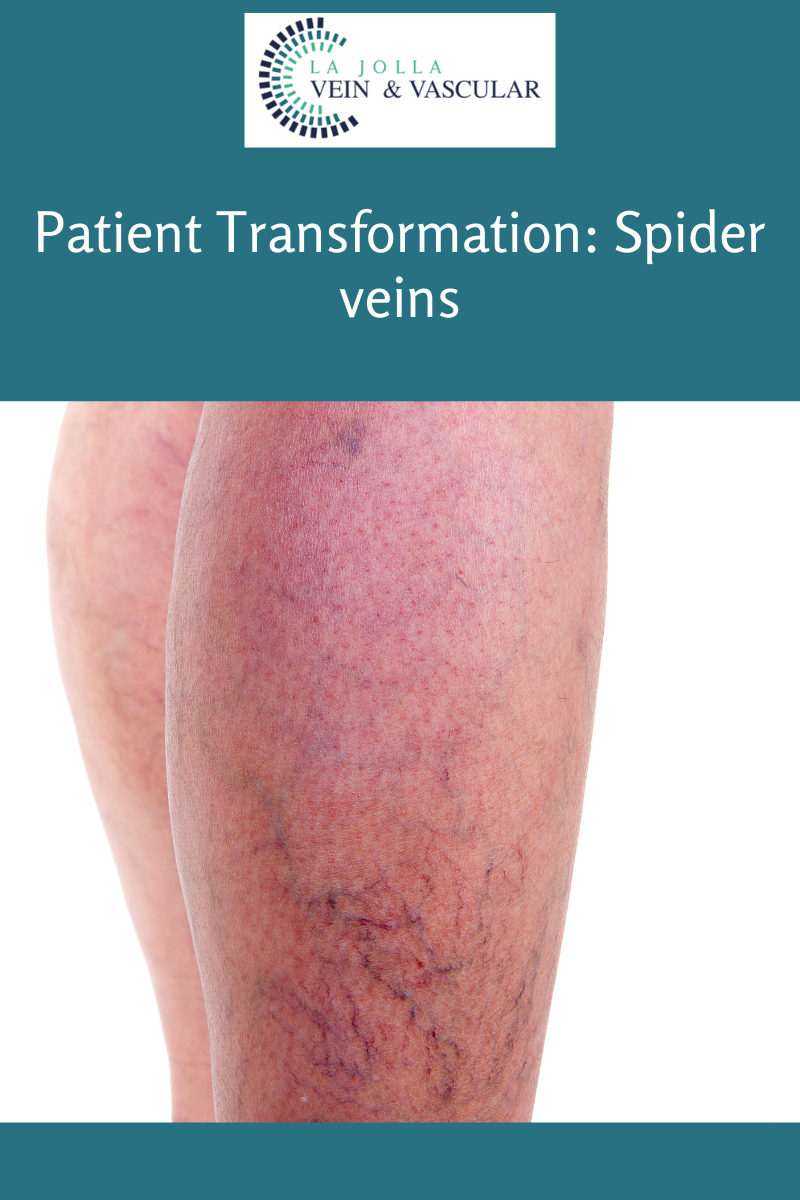
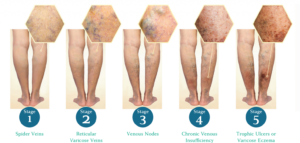
Spider veins are the fine, thread-like reddish veins at the surface of the skin. Spider veins are not healthy. Spider veins are often considered a cosmetic issue, but they can be associated with underlying feeder veins, not visible to the naked eye. Feeder veins are the ‘blue veins’ also known as ‘reticular veins,’ that give rise to spider veins. They may also be a sign of underlying venous insufficiency. For example, spider veins located in the inner ankles and inner thighs can indicate an underlying problem with the saphenous vein. As a result, an ultrasound examination may be recommended to identify and effectively treat the underlying source of the spider veins.
What are the symptoms?
Vein conditions affect people differently. For some, spider veins can be a painless cosmetic concern, and for others they may cause symptoms. The most common symptoms of spider veins are burning, throbbing, and localized pain. They can also feel hot and itchy and bleed.
What causes them?
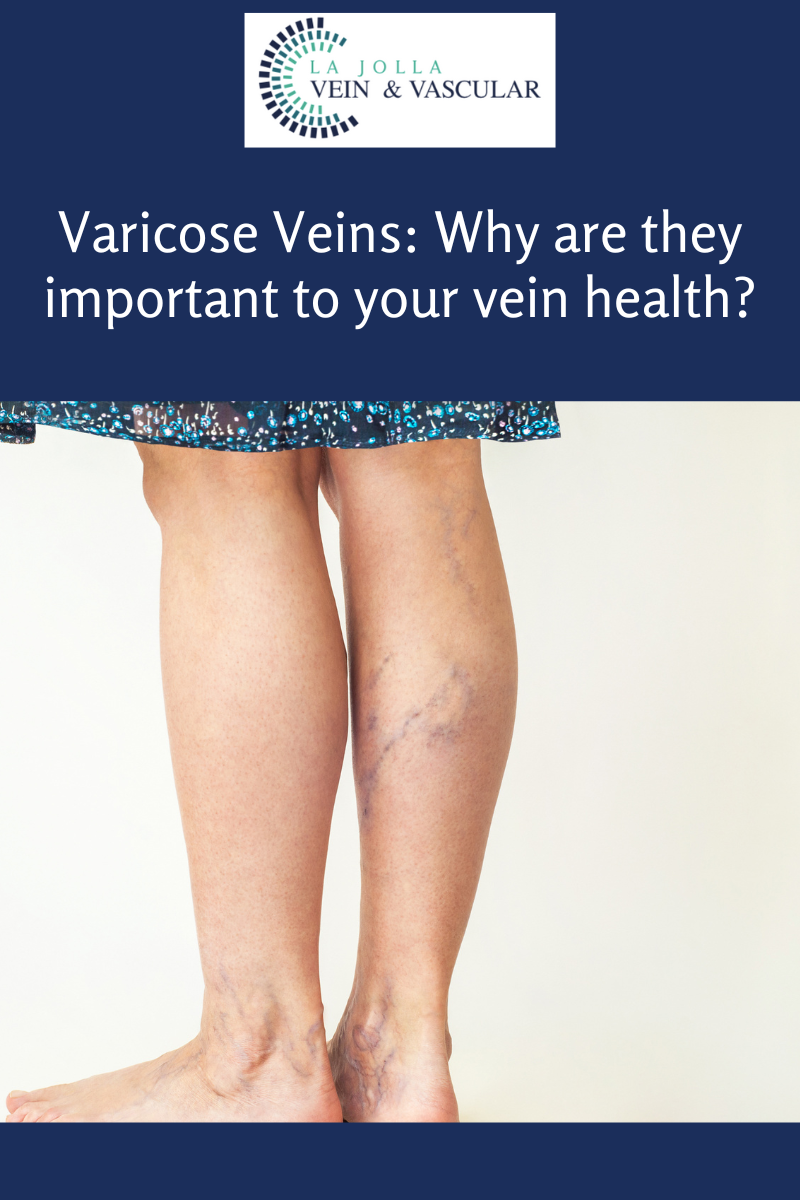
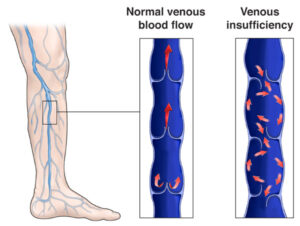
Spider veins in the legs are caused by the same condition that causes varicose veins. Leaky vein valves allow blood to pool within the veins causing them to stretch and become enlarged. Spider veins on other areas of the body, such as the face, and chest can be caused by sun damage, hormone changes or liver disease. Hormones, such as with pregnancy, birth control or hormone replacement therapy can weaken the vein wall.
Risk factors in developing them:
Heredity, gender, age, weight, pregnancy, history of deep vein thrombosis
(DVT and blood clots), standing or sitting for long periods of time, smoking, exposure to heat (hot tubs, baths, saunas), and tight clothing.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!