How does ClariVein® help with vein health?
LJVascular2024-03-06T13:48:21-08:00Exploring the Innovative ClariVein® Procedure: Benefits, Procedure Walkthrough, and More
For those grappling with backward blood flow or “reflux” in their saphenous vein(s), the ClariVein® procedure stands as a promising minimally invasive remedy. In this article, we’ll delve into the mechanics of this groundbreaking treatment and provide insights into what to anticipate on the day of the procedure. Discover how ClariVein® can help restore leg health and significantly improve your quality of life.
Understanding How the Treatment Functions
The ClariVein® procedure is designed to effectively address saphenous vein reflux. This minimally invasive approach takes less than an hour, allowing patients to resume their daily routines on the same day. But how does this innovative treatment function?
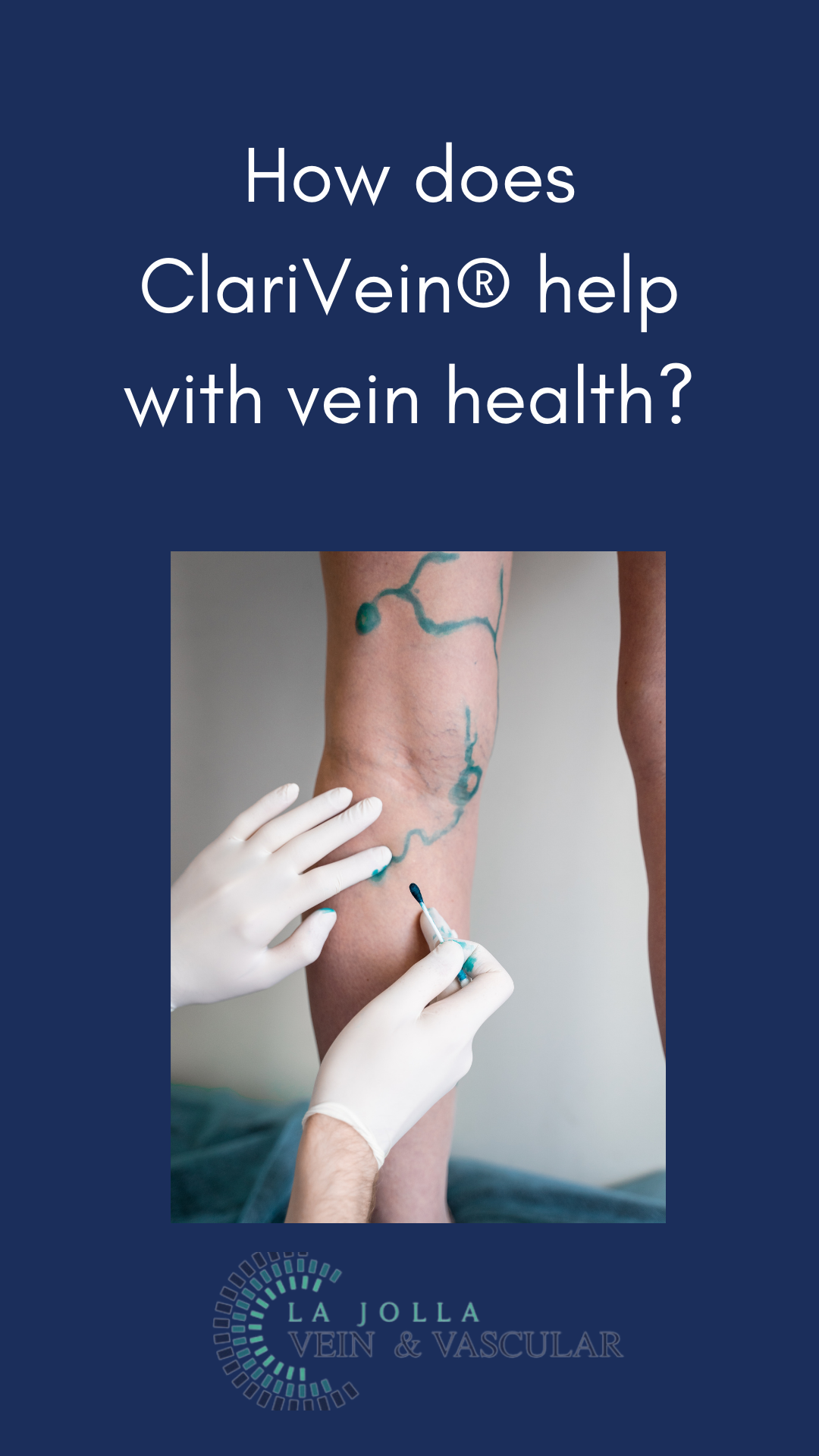
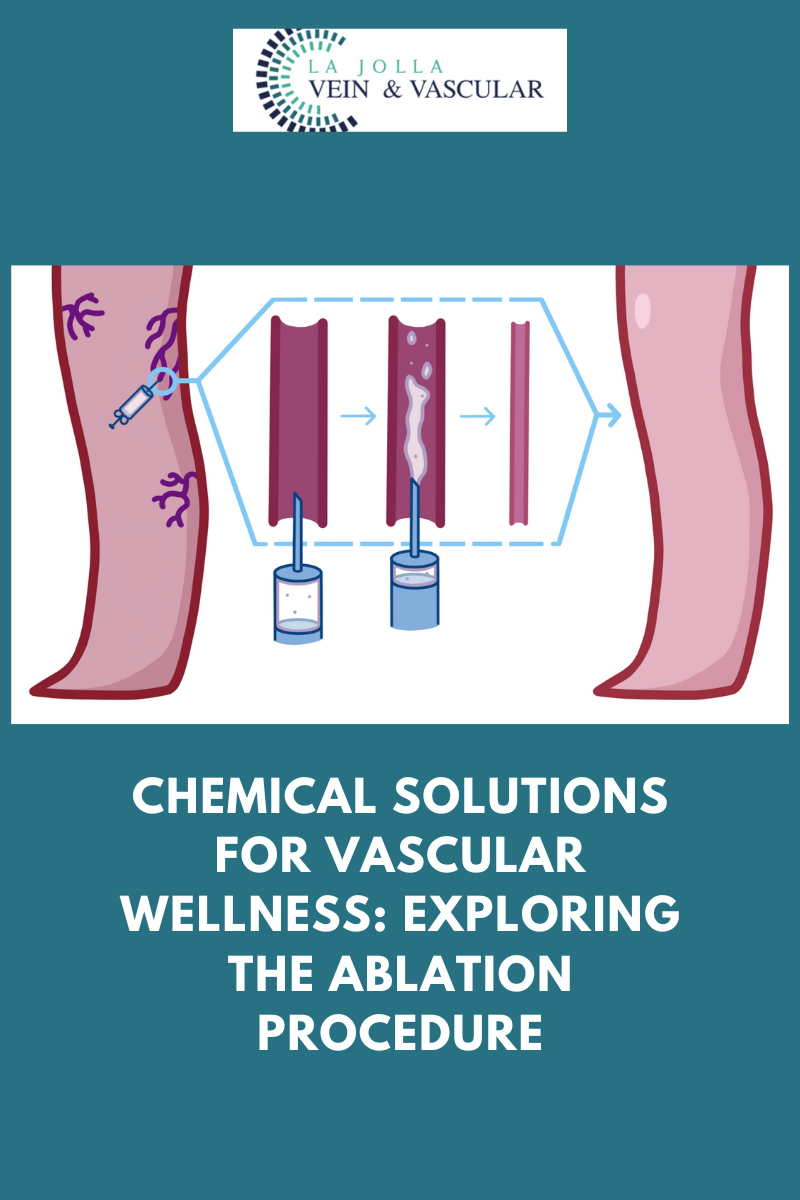
The process commences by numbing the skin with lidocaine. Once the skin is adequately anesthetized, a ClariVein® catheter is cautiously inserted into the affected vein. This catheter executes two crucial treatments:
Mechanical Treatment with a Delicate Rotating Wire: Featuring a small rotating wire, the ClariVein® catheter gently closes the problematic vein. This mechanical treatment is painless yet remarkably effective.
Chemical Treatment using Polidocanol: Alongside the mechanical treatment, the catheter administers polidocanol, a detergent-type sclerosant medication commonly employed in varicose vein treatments. This chemical treatment further contributes to the closure of the vein.
Surprisingly, this technique necessitates only one skin puncture, similar to the placement of an IV. It’s a minimally invasive approach designed to minimize discomfort for patients.
What to Expect on the Treatment Day
Now that you have a clearer understanding of how the ClariVein® procedure operates, let’s delve into what awaits you on the day of your treatment.
Local Anesthesia and Mild Oral Sedative: The procedure is conducted under local anesthesia. Many patients opt to take a mild oral sedative, like Valium, for added relaxation, typically after check-in and paperwork completion.
Comfortable Setup: Upon changing into a gown (leaving your underwear on), you’ll be positioned based on the specific vein to be treated—lying on your back or belly. Special accommodations are arranged for your comfort.
Entertainment Options: To help you relax, you’ll have access to entertainment like watching a movie on Netflix or listening to music during the procedure.
Ultrasound Mapping: Before the treatment begins, the doctor uses ultrasound to map the vein(s) requiring treatment.
Numbing and Puncture: The numbed area of the skin undergoes a tiny puncture to pass the ClariVein® catheter. Lidocaine is injected to ensure a painless process.
Treatment Process: Once the catheter and rotating wire are in place, the doctor initiates the treatment. You might feel a tickling or vibrating sensation, but pain should be minimal to nonexistent.
Compression Stocking: Following the procedure, you’ll be aided in wearing a compression stocking, to be worn continuously for 72 hours.
Post-Procedure Walk: Before departure, you’ll be encouraged to walk for 30 minutes to enhance circulation, further boosting the treatment’s effectiveness.
In Conclusion
The ClariVein® procedure presents a swift, minimally invasive remedy for saphenous vein reflux. By grasping the treatment’s mechanism and anticipating the procedure day, you can approach it confidently. Bid farewell to the discomfort of saphenous vein reflux and usher in a healthier, pain-free future with ClariVein®.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!