Patient Transformation: Varicose Veins
LJVascular2023-05-24T14:01:21-07:00Varicose Vein Treatment: Patient Transformations
What are varicose veins?
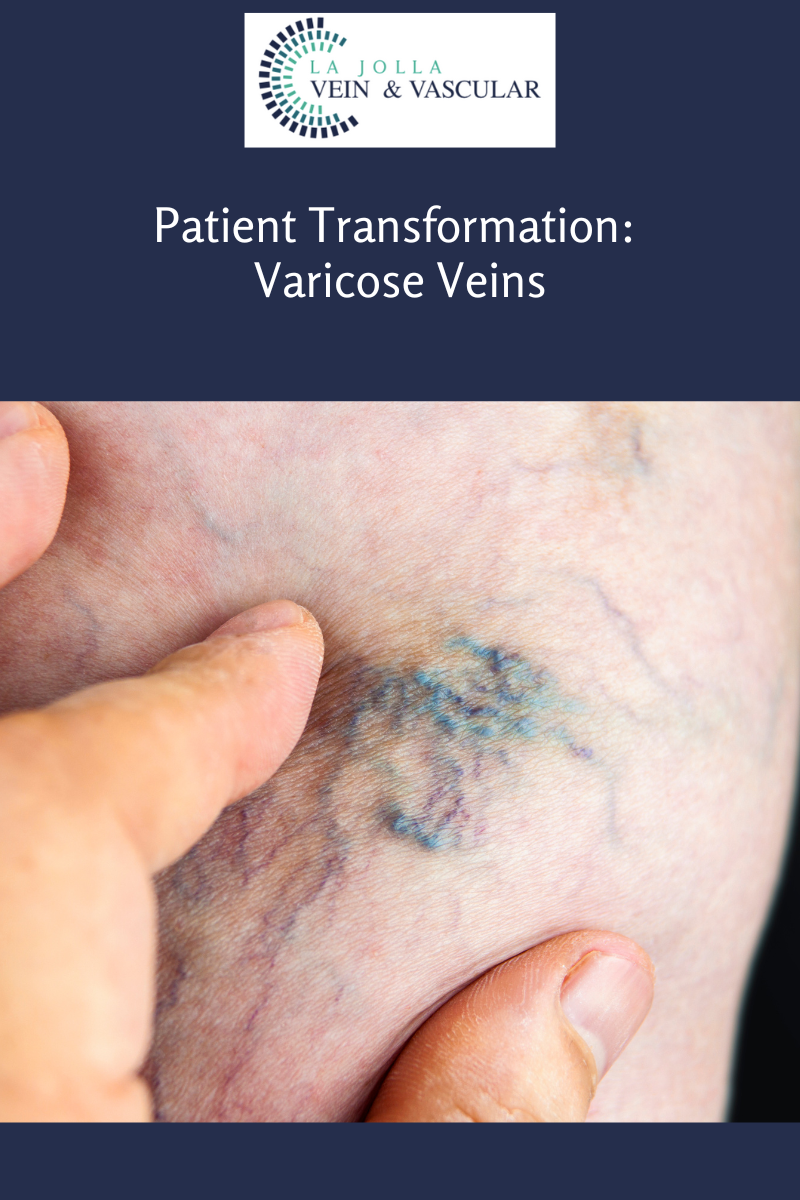
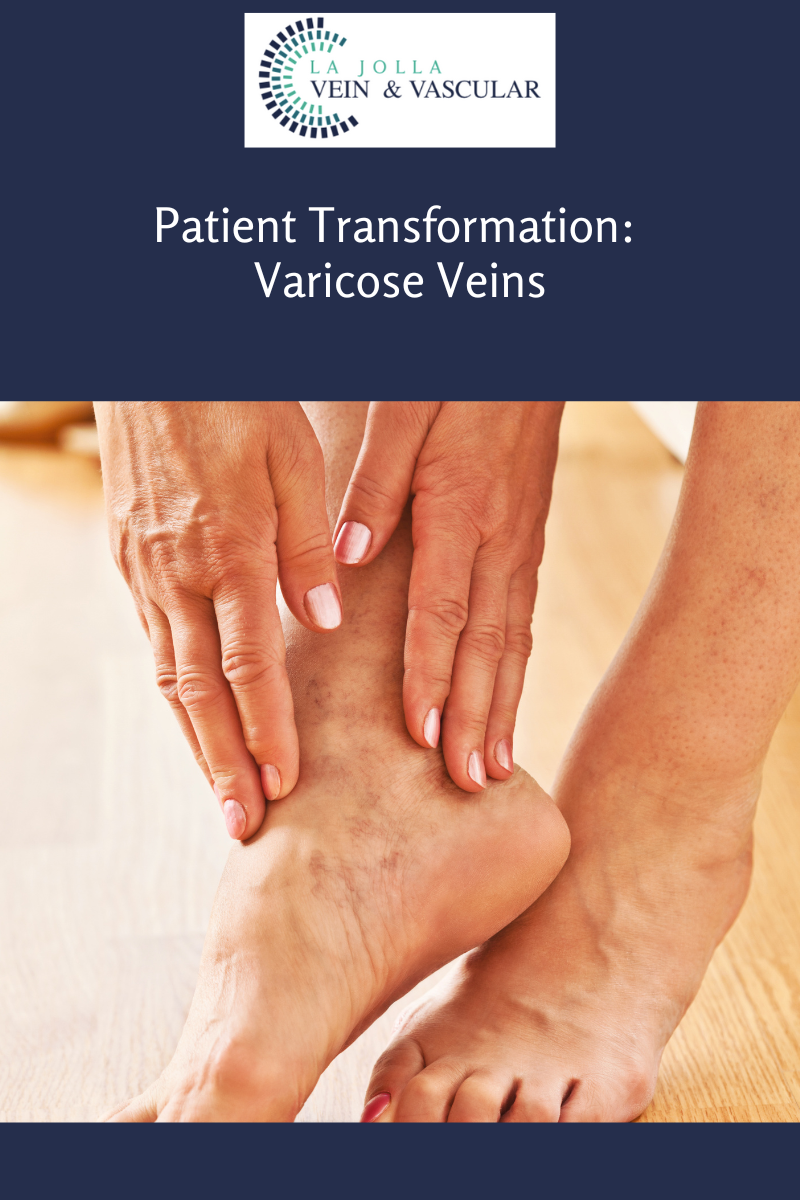
They are the twisted, bulging veins just beneath the surface of the skin. These veins are swollen, twisted veins that you can see just under the surface of the skin. These veins usually occur in the legs, but they also can form in other parts of the body. Varicose veins are a common condition.
What causes them?
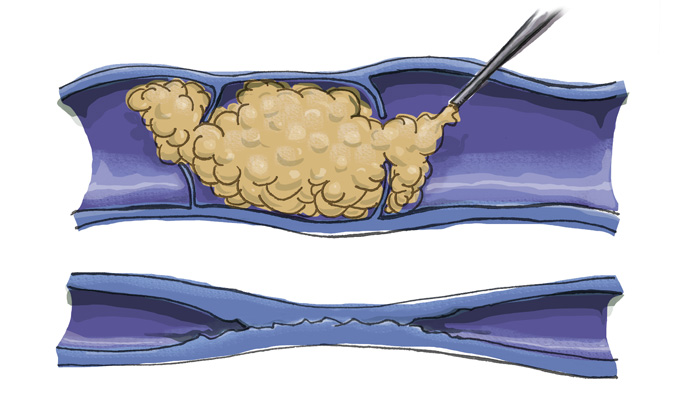
Varicose veins are caused by leaky vein valves, which allow blood to pool within the veins causing them to stretch and become enlarged. These veins can be an isolated finding, but the majority of the time, they are caused by underlying venous reflux disease. Venous reflux disease is also known as venous stasis, venous insufficiency or venous incompetence. Reflux may occur in the deep and/or superficial leg veins.
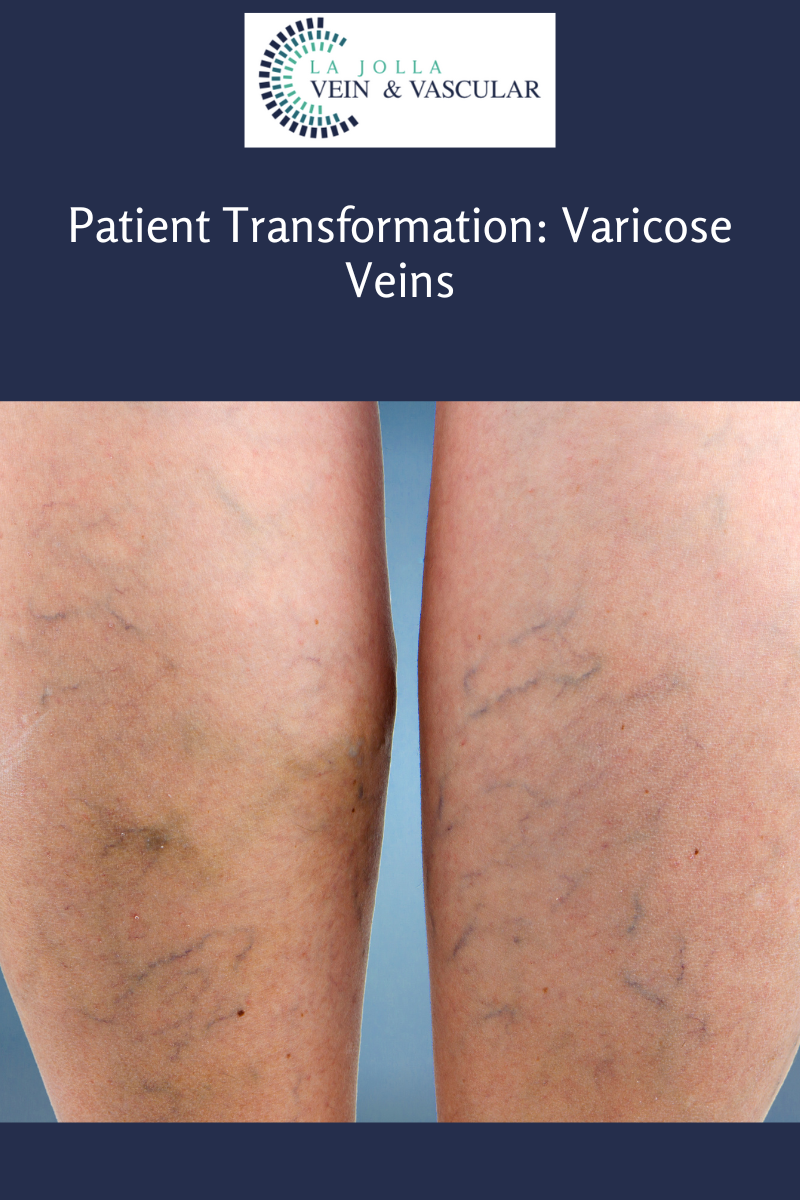
In our study, led by Dr. Nisha Bunke and published in the Journal of Vascular Ultrasound in 2018, we studied over 1,000 legs with varicose veins. Over 90% of the time, the source of the varicose veins were the great and small saphenous veins. The Great Saphenous Vein (GSV) courses up the middle of the thigh and calf and the small saphenous vein (SSV), which courses along the back of the calf. Normally, there are one-way valves within the leg veins, which help blood flow in one direction: toward the heart. This means blood is traveling against gravity. The calf muscle also helps move blood toward the heart. When vein valves are leaky, blood flows backward (reflux) towards the feet. Blood pools in the lower legs, causing bulging veins at the surface.
As you can see below, these patient transformations after varicose vein treatment are remarkable!



“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!