How do I choose the right vein doctor?
LJVascular2024-03-26T15:55:59-07:00Whether you’re seeking treatment for a medical condition or pursuing cosmetic enhancements, selecting the right physician is paramount. When it comes to vein-related issues, such as varicose veins or vascular conditions, making an informed choice can significantly impact your treatment outcomes and overall experience. Here are some essential considerations to keep in mind when choosing a vein doctor:
- Specialization in Vascular Conditions:
Opt for a doctor who specializes in vascular conditions. Venous diseases can be intricate, and expertise in this field ensures accurate diagnosis and effective treatment. Look for a physician with a wealth of experience in dealing with various vein and vascular issues. Avoid those who merely ‘dabble’ in vein treatments, as specialization typically leads to better outcomes and access to the latest treatment options.
- Fellowship Training in Vascular Disease:
Choose a doctor who has undergone fellowship training in vascular disease. While any physician can perform vein procedures, those with additional rigorous training and certification in surgery and vascular specialties are better equipped to address complex issues. Vascular surgeons, in particular, possess comprehensive knowledge and a detailed understanding of vascular problems, making them ideal candidates for vein-related treatments.
- Board Certification:
Ensure that the doctor is board-certified. While all physicians must be licensed to practice medicine, board certification indicates a higher level of expertise and specialization in a particular field. For vein treatments, seek out physicians who hold credentials from reputable vascular boards, such as Sarah Lucas, MD, and Nisha Bunke, MD.
- Facility Accreditation:
Verify if the vein clinic and vascular diagnostic lab are accredited. Accreditation guarantees the quality of equipment and the expertise of personnel conducting diagnostic studies. Choosing an accredited facility ensures that you receive reliable and high-standard care throughout your treatment process.
- Ultrasound Diagnosis by a Registered Vascular Technologist (RVT):
Confirm that ultrasound diagnosis is performed by a Registered Vascular Technologist (RVT). Accurate ultrasound imaging is crucial for diagnosing venous diseases effectively. A skilled vascular sonographer, coupled with a doctor trained to interpret the studies, ensures precise diagnosis and tailored treatment plans.
- Comfort Level with the Doctor and Facility:
Lastly, trust your instincts and assess your comfort level with both the doctor and the facility. Establishing a rapport with your provider is essential for effective communication and mutual understanding. Choose a facility that is not only state-of-the-art but also welcoming, with provisions for after-hours support if needed.
In conclusion, selecting a vein doctor requires careful consideration of various factors, ranging from specialization and credentials to facility accreditation and personal comfort. By prioritizing these aspects, you can ensure that you receive optimal care and achieve the best possible outcomes for your vein-related concerns. Take your time, do your research, and make an informed decision that aligns with your specific needs and preferences. Your vein health deserves nothing less than the highest standard of care.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
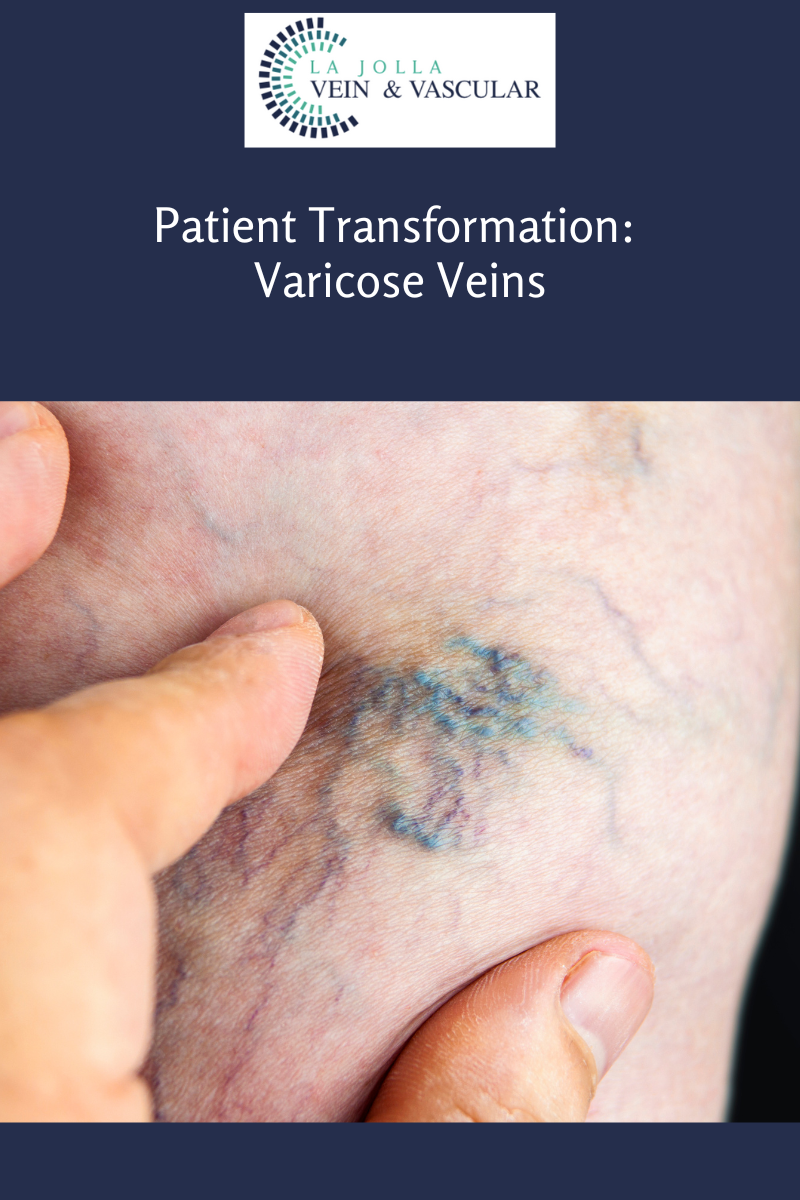
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!