Boost Your Confidence: Exploring Cosmetic Sclerotherapy for Radiant, Healthy Legs
LJVascular2023-12-26T16:38:18-08:00Boost Your Confidence: Exploring Cosmetic Sclerotherapy for Radiant, Healthy Legs
Cosmetic sclerotherapy stands as a highly recommended and successful treatment for spider veins and reticular veins in the legs. This article delves into the specifics of sclerotherapy, highlighting its advantages over other treatments, offering insights into the treatment process, and outlining the path toward achieving optimum results. Whether you’re contemplating this procedure or seeking to broaden your knowledge about it, read on to discover how sclerotherapy can bid farewell to unsightly spider veins, uplifting your confidence along the way.
Understanding Sclerotherapy
Sclerotherapy represents a well-established technique for addressing spider veins. It entails injecting medication directly into the affected vein, prompting it to collapse and gradually fade away. While sclerotherapy has a long history of use, modern solutions like Asclera™ have made the process more comfortable, enabling an immediate return to regular activities.
Advantages of Sclerotherapy:
Enhanced Comfort: Contemporary solutions like Asclera™ have minimized discomfort, rendering sclerotherapy more tolerable for patients compared to older saline-based methods.
Targeted Treatment: Unlike laser therapies that might overlook underlying ‘feeder veins,’ sclerotherapy is favored by many vein specialists for its efficacy in addressing these crucial veins.
Multiple Sessions for Optimal Outcomes: Achieving optimal results often necessitates more than one treatment session, typically ranging from 2 to 5 sessions spaced a month apart. Your healthcare provider will customize a treatment plan tailored to your needs.
Post-Treatment Care: Wearing compression stockings after treatment bolsters results, ensuring a gradual fading of the treated veins.
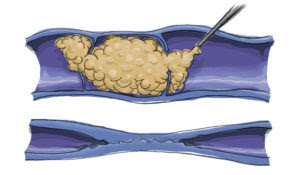
Foam Sclerotherapy for Larger Veins
For larger veins such as varicose veins, a specialized form of sclerotherapy, known as foam sclerotherapy, is employed:
Foamed Solution: Unlike liquid solutions, foam sclerotherapy utilizes a foamed solution injected directly into the vein through a fine needle.
Ultrasound Monitoring: Precise and painless delivery of the foamed solution into nearby varicose veins is achieved through ultrasound monitoring. This process effectively seals the veins shut, and over time, the body naturally breaks down and absorbs these sealed veins.
What to Expect During Your Treatment Days
Your treatment days typically involve a straightforward process:
Consent and Attire: Starting with signing a consent form, you’ll change into shorts provided by the office for easy access to the treated areas.
Skin Preparation: Your skin will be meticulously cleaned with alcohol to maintain a sterile environment for the procedure.
Injection Procedure: The sclerosant medication will be delicately injected into your veins using a fine needle.
Compression Stockings: Post-treatment, you’ll be assisted in wearing compression stockings.
Post-Treatment Walk: To optimize results, you’ll be encouraged to walk for 30 minutes before departing. Some temporary achiness and tenderness in your legs post-treatment are normal.
Sclerotherapy, whether for spider veins or larger varicose veins, remains a trusted and effective vein treatment. Its minimal discomfort, precise targeting of feeder veins, and focus on patient comfort position it as a preferred choice among vein specialists. Whether you’re contemplating or have already decided on sclerotherapy, you’re well on your way to relishing healthier, vein-free legs, and a renewed sense of confidence.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!